Differential Diagnosis Of Orofacial Pain Notes
Pain is an unpleasant, subjective, sensational, and emotional experience associated with actual or potential tissue damage. Orofacial pain is the field of dentistry related to the diagnosis and management of chronic, complex facial pain and orofacial disorders.
Table of Contents
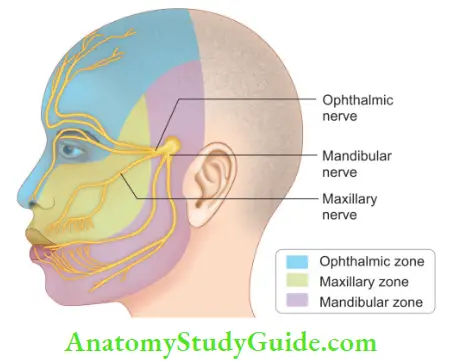
Orofacial pain, like pain elsewhere in the body, is usually the result of tissue damage and the activation of nociceptors, which transmit a noxious stimulus to the brain. Orofacial disorders are complex and difficult to diagnose due to rich innervations in the head, face, and oral structures.
Read And Learn More: Endodontics Notes
In order to establish a proper diagnosis, one should take a detailed subjective description of pain including quality, intensity, duration, frequency, and periodicity of the pain.
Definition
- Dorland’s Medical Dictionary defines pain as “A more or less localized sensation of discomfort, distress or agony resulting from the stimulation of nerve endings.” It indicates that pain is a protective mechanism against injury.
- The International Association for Study of Pain (IASP) defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
Basically, pain has the function of a warning to tissue damage and activation of a defensive mechanism with the aim of prevention of further damage.
Diagnosis
To establish the correct diagnosis, the clinician must record all relevant information regarding signs, symptoms, history of the present complaint, and past medical and dental history.
History of Pain:
History is an important part of diagnosis; it should assess the present nature and site of pain, along with its causative and aggravating factors. It includes:
Chief Complaint:
- Location
- Onset
- Chronology
- Quality
- Intensity
- Aggravating factors
- Precipitating factors
- Past medical and dental history
- Psychological analysis
- Review of systems
Location:
By knowing the patient’s description about the location of pain, the clinician should determine whether it is the true source of pain or referred pain.
Onset:
One should know the conditions associated with the initial onset of pain. It may facilitate in recognizing the etiology of pain.
Chronology:
The chronology of pain should be recorded in the following pattern:
- Initiation
- Clinical course:
- Mode
- Periodicity
- Frequency
- Duration
Quality:
It tells how pain is felt to the patient, for example,
- Dull, gnawing, or aching
- Throbbing, pounding, or pulsating
- Sharp, recurrent, or stabbing
- Squeezing or crushing
Intensity:
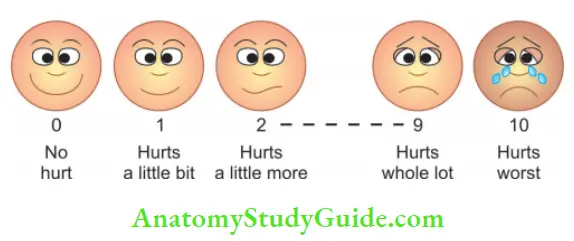
The intensity of pain is established by distinguishing mild, moderate, and severe pain. A visual analog scale is used to assess the intensity of pain. The patient is given a line on which no pain is written at one end and severe at another end. The scale has markings from 0 to 10, where 0 indicates no pain and 10 as maximum pain.
- Pain index : 0–10
- Pain classifiation :Mild, Moderate, Severe
Aggravating Factors:
Aggravating factors can be local or conditional. Local factors can be irritants like heat, cold, sweets, sour and pain on biting, etc. Conditional factors can be changes of posture, physical activities, and hormonal changes.
Orofacial Pain
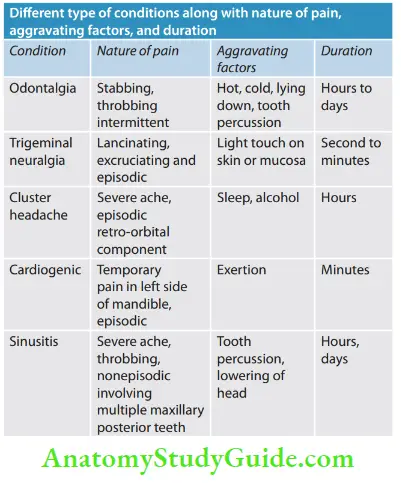
Orofacial pain can be divided into odontogenic (dental pain) and nonodontogenic pain (nondental). Dental pain may originate from pulpal or periradicular tissue. Nondental pain can be in the form of myofascial toothache, vascular headache, cluster headache, sinusitis, and trigeminal neuralgia.
Sources Of Odontogenic Pain
Dental Pain of Pulpal Origin:
Pulpal pain is of threshold type, that is, no response occurs until the threshold level is increased. The pulp may respond to chemical, mechanical, electrical, or thermal stimulation but not to ordinary masticatory functions. In healthy pulp, sensitivity produced by cold and warm stimuli lasts for 1–2 s.
Since the pulp does not contain proprioceptors, pulpal pain cannot be localized by the patient.
Dental Pain of Periodontal Origin:
Periodontal pain is deep somatic pain of the musculoskeletal type. In the periodontal ligament (PDL), proprioceptors are present which allow precise localization of pressure stimuli so that the patient can localize pain of periodontal origin. This localization can be identifid by applying pressure to the tooth axially and laterally.
Sources of odontogenic pain
- Pulpal pain
- Dentinal sensitivity
- Reversible pulpitis
- Irreversible pulpitis
- Necrotic pulp
- Periodontal pain
- Symptomatic apical periodontitis
- Acute periapical abscess
- Asymptomatic apical periodontitis
- Periodontal abscess
- Pericoronitis
Pulpal Pain
Dentinal Sensitivity:
According to Holland et al., dentin hypersensitivity is characterized as a short, sharp pain arising from exposed dentin in response to stimuli typically thermal, evaporative, tactile, osmotic, or chemical, and which cannot be ascribed to any other form of dental pathology.
It is caused by a disturbance in fluid flow present in dentinal tubules which stretches or compresses the nerve endings that pass alongside the tubular extensions of odontoblasts.
Dentinal Sensitivity Diagnosis:
- Pain is the most common feature which can range from mild to severe
- The most commonly involved teeth are the buccal surfaces of premolars and labial surfaces of incisors
- Stimuli causing pain can be thermal (hot and cold), mechanical (toothbrush), osmotic (sweet foods), and acidic (sour and citric juices) stimuli
Dentinal Sensitivity Treatment:
The main principles of treatment are to plug the dentinal tubules preventing the fluid flow and desensitize the nerve, making it less responsive to stimulation. It is done by application of dentifrices, in office products like varnishes and sealants, etc.
Reversible Pulpitis:
In reversible pulpitis, short and sharp pain occurs that lasts only when stimuli is applied. On removal of stimuli, pain ceases within 1–2 s. Etiology can be caries, faulty restoration, trauma, or recent restorative procedures.
Reversible Pulpitis Diagnosis:
Diagnosis is made by careful history and clinical examination. Short and sharp pain disappears on the removal of stimuli. Pain is usually caused by cold, sweet, or sour things. Since the pulp is especially sensitive to cold stimuli, the cold test is the best method to diagnose the case.
Reversible Pulpitis Differential Diagnosis:
Reversible pulpitis can be differentiated from irreversible pulpitis by the character of pain, and thermal and electric pulp tests.
Reversible Pulpitis Treatment:
- Removal of the cause if present (caries, fractured restoration, exposed dentinal tubules)
- If a recent operative procedure or trauma has taken place, then postpone the additional treatment and observe the tooth
- If pulp exposure is detected, go for a root canal treatment
Irreversible Pulpitis:
Irreversible pulpitis develops if the inflammatory process progresses to involve pulp. The patient may have a history of spontaneous pain or exaggerated response to hot or cold that lingers even after the stimulus is removed. The involved tooth usually presents extensive restoration and/or caries.
Irreversible Pulpitis Diagnosis:
Diagnosis is usually made after taking a thorough history and clinical examination of the patient.
- The patient usually gives a history of spontaneous pain
- The tooth is hypersensitive to hot or cold that is prolonged in duration
- The pulp may be vital or partially vital
- In certain cases of irreversible pulpitis, the patient may arrive at the dental clinic with a glass of ice/cold water. In these cases, cold actually alleviate the patient’s pain and, thus, can be used as a diagnostic test. Cooling of the dentin and the resultant contraction of the flid in the tubules relieves the pressure on pulpal nerve fiers caused by edema and inflammation of the pulp
Irreversible Pulpitis Differential Diagnosis:
- Reversible pulpitis at an early stage
- In case of the symptomatic stage, it may resemble an acute alveolar abscess
Irreversible Pulpitis Treatment:
Complete removal of pulpal tissue should be done, that is, endodontic therapy.
Necrotic Pulp:
It results from the continued degeneration of an acutely inflamed pulp. The literal meaning of necrosis is death, that is, the pulpal tissue becomes dead because of untreated pulpal inflammation. In pulpal necrosis, there is a progressive breakdown of cellular organization with no reparative function.
It is frequently associated with apical radiolucent lesions. In the case of multirooted teeth, one root may contain partially vital pulp, whereas other roots may be nonvital.
Necrotic Pulp Diagnosis:
- The tooth is usually asymptomatic, and may give moderate to severe pain on biting pressure (it is not a symptom of necrotic pulp but it indicates inflammation)
- Pulp tests show negative responses but in the case of multirooted teeth, it can give false positive results.
Necrotic Pulp Treatment:
Complete removal of pulpal tissue that is root canal treatment.
Periodontal Pain
Symptomatic Apical Periodontitis:
It is the inflammation of the periodontal ligament which is caused by tissue damage, an extension of pulpal pathology, or occlusal trauma. The tooth may be elevated out of the socket because of the built-up fluid pressure in the periodontal ligament. Pain remains until the bone is resorbed, fluid is drained, or irritants are removed.
symptomatic Apical Periodontitis Diagnosis:
- Check for decay, fracture lines, swelling, hyper occlusion, or sinus tracts
- The patient has moderate to severe pain on the percussion
- Mobility may or may not be present
- Pulp tests are essential and their results must be correlated with other diagnostic information in order to determine if inflammation is of pulpal origin or from occlusal trauma
- Radiographs may show no change or widening of periodontal ligament space in some cases
Symptomatic Apical Periodontitis Differential Diagnosis:
It should be differentiated from the acute alveolar abscess. The patient’s history, symptoms, and clinical tests help in differentiating it from a periodontal abscess
Symptomatic Apical Periodontitis Treatment:
- Complete removal of pulp
- Occlusal adjustment
Acute Periapical Abscess:
An acute periapical abscess is an acute inflammation of periapical tissue characterized by a localized accumulation of pus at the apex of a tooth. It is a painful condition that results from an advanced necrotic pulp. Patients usually relate previous painful episodes from irreversible pulpitis or necrotic pulp. Swelling, tooth mobility, and fever are seen in advanced cases.
Acute Periapical Abscess Diagnosis:
- Spontaneous dull, throbbing, or persistent pain is present
- The tooth is extremely sensitive to percussion
- Mobility may be present
- On palpation, the tooth may be sensitive
- Vestibular or facial swelling in seen in these patients
- Pulp tests show negative results
Acute Periapical Abscess Differential Diagnosis:
Pulp vitality tests help in reaching the correct diagnosis
Acute Periapical Abscess Treatment:
- Drainage
- Complete extirpation of pulp
- Appropriate analgesics and antibiotics if necessary
Chronic Apical Periodontitis:
It is caused by necrotic pulp which results from prolonged inflammation that erodes the cortical plate making a periapical lesion visible on the radiograph. The lesion contains granulation tissue consisting of fibroblasts and collagen.
Chronic Apical Periodontitis Diagnosis:
- It is usually asymptomatic but in the acute phase may cause a dull, throbbing pain
- Pulp tests show nonvital pulp
- There is no pain on the percussion
- Radiographically, it is usually associated with periradicular radiolucent changes
Chronic Apical Periodontitis Differential Diagnosis:
It can be diffrentiated on the basis of histopathological features
Periodontal Abscess:
An acute periodontal abscess is a virulent infection of an existing periodontal pocket. It can also occur because of apical extension of infection from the gingival pocket.
Chronic Apical Periodontitis Diagnosis:
- The tooth is tender to lateral percussion
- When the sinus tract is traced using gutta-percha, it points toward the lateral aspect of the tooth
Chronic Apical Periodontitis Treatment:
Root planing and curettage.
Pericoronitis:
It is inflammation of the periodontal tissues surrounding the erupting third molar.
Pericoronitis Diagnosis:
- Deep pain which radiates to the ear and neck
- May be associated with trismus
Pericoronitis Treatment:
Operculectomy and surgical removal of the tooth if required.
Sources Of Nonodontogenic Pain
As dental pain is considered one of the most common causes of orofacial pain, the dentist can be easily drawn to the diagnosis of pain of odontogenic origin. There are many structures in the head and neck region which can simulate dental pain. Such types of pain are classified under heterotrophic pain. Heterotrophic pain can be defined as any pain felt in an area other than its true source.
There are three general types of pain:
- Central pain
- Projected pain
- Referred pain
Referred Pain:
Referred pain is a heterotrophic pain that is felt in an area innervated by a different nerve, from one that mediates the primary pain. Referred pain is wholly dependent upon the original source of pain.
It cannot be provoked by stimulation where the pain is felt while it can be accentuated only by stimulation in the area where the primary source of pain is present. Referred pain can be of odontogenic or nonodontogenic origin.
Odontogenic Referred Pain:
In this, pain originates from endodontically involved tooth and is referred to adjacent teeth/tooth or approximating deep and superficial structures. For example, pain from pulpal involvement of the mandibular second or third molar is referred to ear. This pain is diagnosed by selective anesthesia technique.
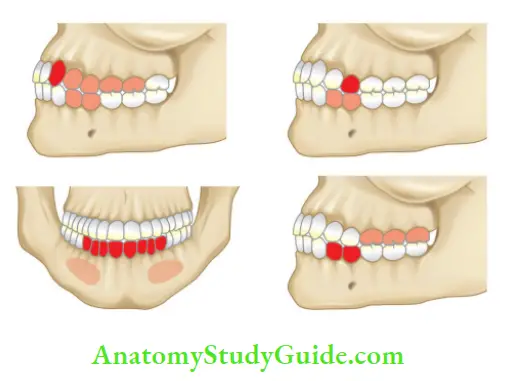
Nonodontogenic Referred Pain:
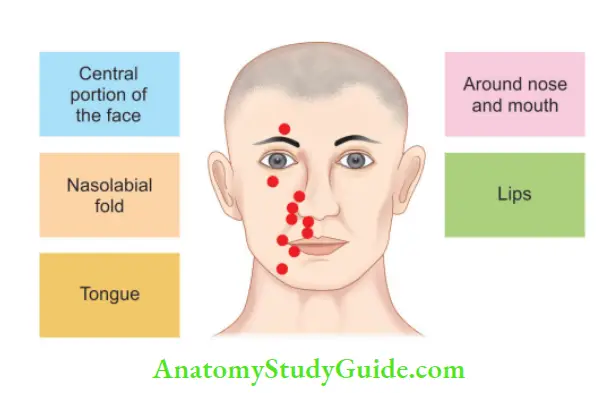
In this, pain originates from deep tissues, muscles, joints, ligaments, etc., and is perceived at a site away from its origin. Pain arising from musculoskeletal organs is deep, dull, aching, and diffused type. Pain from cutaneous origin is sharp, burning, and localized (for example, pain of maxillary sinusitis and may result in pain in maxillary premolars).
Myofascial Pain:
It is characterized by chronic pain which occurs during dental procedures, and blows to the mandible. Characteristics of this pain are unilateral, muscle tenderness, presence of clicking sound, and limitation of jaw functions. The most commonly affected muscles are the masseter and temporalis.
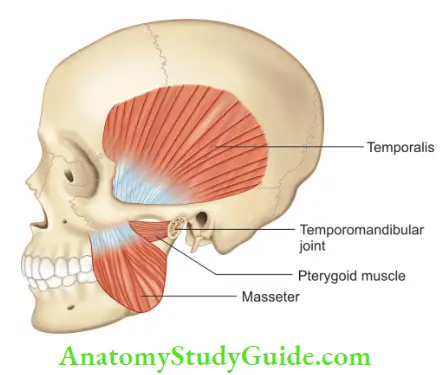
Characteristic Findings of Muscular Toothache:
- Nonpulsatile, diffuse, dull, and constant pain
- Pain increases with the function of masticatory muscles. For example, pain is increased on chewing because of the effect on masseter muscle
- Palpation of the involved muscles at specific points (trigger points)* may induce pain
- Usually arise with or without pulpal or periarticular pathology
- Tooth pain is not relieved by anesthetizing the tooth; rather local anesthesia given at the affected muscle may reduce the toothache
Diagnosis:
These muscular pains as the nonodontogenic tooth is purely based on a lack of symptoms after diagnostic tests such as pulp testing, percussion, and local anesthesia block. Several therapeutic options used in the management of muscular pain are:
- Restriction of functional activities within the painless limit
- Occlusal rearrangement
- Deep massage
- Spray and stretch technique
- Ultrasound therapy
- Local anesthesia at the site of trigger points
- Analgesics
Neurovascular Toothache:
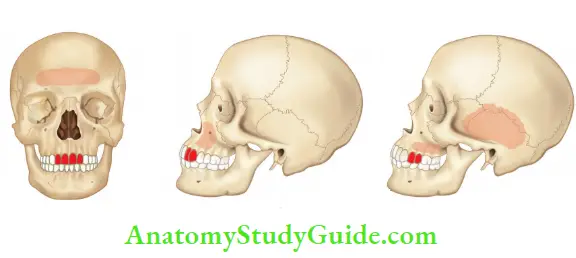
The most common neurovascular pain in the mouth and face is migraine. This category of pain includes three subdivisions of primary headache. These are:
- Migraine
- Tension-type headache
- Cluster headache
These neurovascular entities can produce relatively localized pains that match with the signs and symptoms with the toothache. These accompanying toothaches are usually mistaken for true odontogenic pains and can be treated as separate entities.
Features of Neurovascular Toothache
- Pain is deep, throbbing, spontaneous in onset, variable in nature, and pulsatile. These are characteristics which simulate pulpal pain
- Pain is predominantly unilateral
- Accompanying toothache shows periods of remission that imitate the pain-free episodes or temporal behavior found in neurovascular pain
- Headache is considered as the main symptom. It is most often accompanied by toothache
- Recurrence is a characteristic finding in neurovascular pain. Sometimes, the pain may undergo remission after dental treatment has been performed in these teeth. It usually appears for a certain period of time and may even spread to adjacent teeth, opposing teeth, or the entire face
- Autonomic effects such as nasal congestion, lacrimation, rhinorrhea, and edema of the eyelids and face are seen. Sometimes edema of the eyelids and face might lead to confusion in diagnosis as these features bear a resemblance to abscess
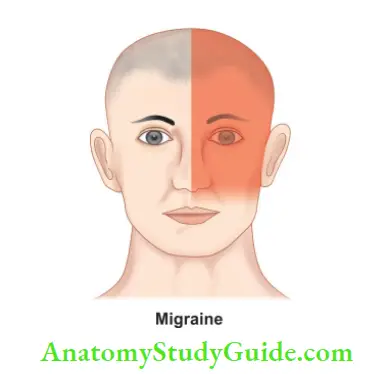
Migraine:
Migraine has been divided into two main types:
- Migraine with aura
- Migraine without aura
Features of Migraine:
- Commonly found between the age group 20–40 years
- Visual auras are the most common. These usually occur 10–30 min prior to the onset of headache pain (migraine with aura)
- Pain is usually unilateral, pulsatile, or throbbing in nature
- More common in females
- The patient usually experiences nausea, vomiting, photophobia
- Various drugs used in the management of migraine are sumatriptan, β-blockers, tricyclic antidepressants, and calcium channel blockers
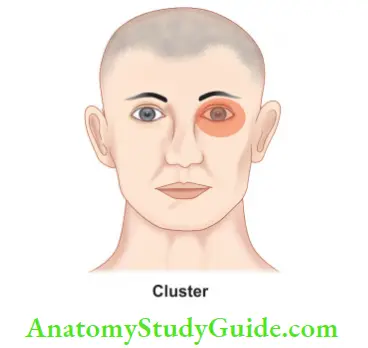
Cluster Headache:
- Commonly found in the age group 20–50 years
- Cluster headaches derive their name from the temporal behavior and usually occur in series, that is, one to eight attacks per day
- More common in males than females
- Pain is unilateral, excruciating, and continuous in nature and usually found in the orbital, supraorbital, or temporal region
- Autonomic symptoms such as nasal stuffiness, lacrimation, rhinorrhea, or edema of eyelids and face are usually found
- Standard treatment is the inhalation of 100% oxygen
The behavior of neurovascular variants should be well appreciated to avoid any unnecessary treatment and frustration felt by the patient and clinician. Although the term neurovascular toothache is nondescriptive, it has given the dentist an important clinical entity that has been misdiagnosed and mistreated in the past.
Signs and symptoms of neurovascular headache that mimic the toothache are:
- Periodic and recurrent nature
- Precise recognition of painful tooth
- Absence of local dental etiology
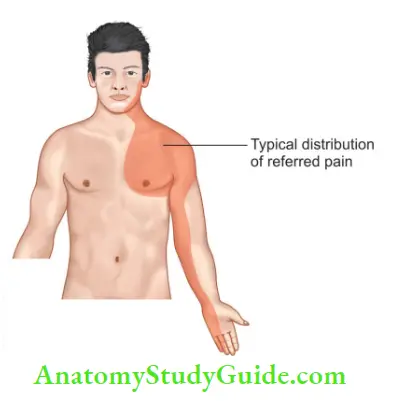
Cardiac Toothache:
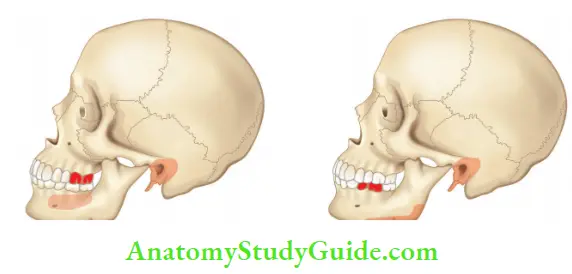
Excruciating referred pain felt in the mandible and maxilla from an area outside the head and neck region is most commonly from the heart. Cardiac pain is clinically characterized by heaviness, tightness, or throbbing pain in the substernal region which commonly radiates to the left shoulder, arm, neck, and mandible.
Characteristics of cardiac toothache are:
- Pain is of sudden in onset, gradually increasing in intensity, diffuse with a cyclic pattern that varies in intensity from mild to severe
- Tooth pain is increased with physical activities
- Chest pain is usually associated
- Pain is not relieved by anesthesia of the lower jaw or by giving analgesics
Neuropathic Pain:
Neuropathic pain is usually caused by abnormalities in the neural structures themselves. Neuropathic pain is sometimes misdiagnosed as psychogenic pain because local factors cannot be visualized.
Neuropathic pain can be classified into different categories:
- Neuralgia
- Neuritis
- Neuropathy
1. Neuralgia
Paroxysmal, unilateral, severe, stabbing, or lancinating pains usually are the characteristics of all paroxysmal neuralgias. Pain is usually of short duration and lasts for a few seconds.
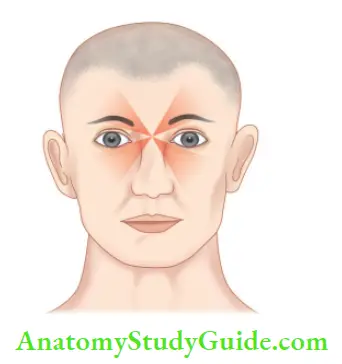
Trigeminal neuralgia:
- It is also known as “tic douloureux” which has a literal meaning of painful jerking
- Usually characterized by paroxysmal, unilateral, sharp, lancinating pain typically confined to one or more branches of the cranial nerve
- Even slight stimulation of “trigger points” may elicit sharp, shooting pain. Sometimes trigger points are present intraorally. These are stimulated upon chewing which may lead to a diagnosis of odontogenic pain. Intraoral trigger points always create confusion in diagnosis if not properly evaluated
- Local anesthesia given at the trigger point reduces the attacks
- It rarely crosses the midline
- Commonly seen in patients over the age of 50 years
- Attacks generally do not occur at night
- The absence of dental etiology along with symptoms of paroxysmal, sharp, shooting pain always alert the dentist to include neuralgia in differential diagnosis
- Treatment includes surgical and medicinal. Usually, the medicinal approach is preferred. It includes administration of carbamazepine, baclofen, phenytoin sodium and gabapentin, etc.
2. Neuritis
Neuritis literally means inflammation of the nerve. It is usually observed as heterotopic pain in the peripheral distribution of the affected nerve. It may be caused by traumatic, bacterial, and viral infections. In neuritis, the inflammatory process elevates the threshold for pricking pain but lowers it for burning pain.
Characteristics of pain in neuritis are:
- Pain has a characteristic burning quality along with easy localization of the site
- It may be associated with other sensory effects such as hyperesthesia, hypoesthesia, paresthesia, dysesthesia, and anesthesia
- Pain is nonpulsatile in nature
- Pain may vary in intensity
Peripheral neuritis is an inflammatory process occurring along the course of never trunk secondary to traumatic, bacterial, thermal, or toxic causes. Neuritis of the superior dental plexus has been reported when inflammation of the sinus is present. Dental nerves frequently lie just below the lining mucosa or are separated by a very thin osseous structure. These nerves are easily involved due to direct extension.
Symptoms usually seen along with antral disease are pain, paresthesia, and anesthesia of a tooth, gingiva, or area supplied by the infraorbital nerve. Mechanical nerve trauma is more common in oral surgery cases. It usually arises from inflammation of the inferior dental nerve either due to trauma or infection.
Acute neuritis cases are always misdiagnosed and remain untreated. Most of the time, dental procedures are done to decrease the symptoms of neuritis as these are difficult to diagnose. These unnecessary dental procedures further act as aggravating factors for neuritis, making it chronic.
Treatment of neuritis:
- Treatment is based on its etiology
- If the bacterial source is present, antibiotics are indicated
- If a viral infection is suspected, antiviral therapy should be started
- If there is no infection, steroids should be considered
3. Neuropathy
This is the term used for localized and sustained pain secondary to an injury or change in neural structure. Atypical odontalgia has been included in neuropathy. Atypical odontalgia means toothache of unknown cause. It is also known as “phantom tooth pain” or “dental migraine.” Most patients who report atypical odontalgia usually have multiple dental procedures completed before reaching a final diagnosis.
Clinical characteristics of neuropathy:
- Also called atypical odontalgia
- More common in women
- Frequently found in the fourth or fifth decades of life
- Tooth pain remains constant or unchanged for weeks or months
- A constant source of pain in the tooth with no local etiology
- The pain usually felt in these patients is dull, aching, and persistent
- The most commonly affected teeth are maxillary premolar and molar region
- Response to local anesthesia is equal in both pulpal toothache and atypical odontalgia
Sinus Toothache:
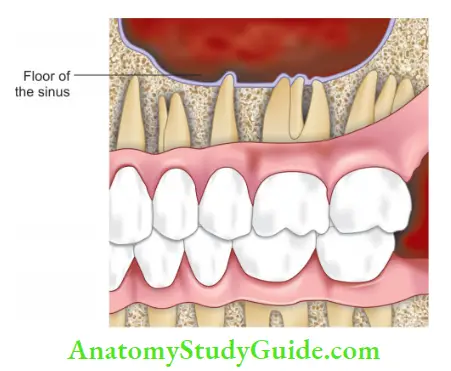
Sinus and nasal mucosal pain is also another source which can mimic a toothache. It is usually expressed as pain throughout the maxilla and maxillary teeth. The patient often complains of pain behind the forehead and/or cheeks.
Clinical characteristics of sinus or nasal mucosal toothache are:
- Fullness or pressure below the eyes. Sinus pressure can cause tooth pain, especially in maxillary molars. The roots of the maxillary molars lie next to the maxillary sinus. Blood vessels and nerves which enter in apical foramina of the molar may run right through the sinus to get into the tooth. Any pressure or inflammation in the sinuses can irritate these nerves resulting in sinus toothache
- Increased pain sensation when the head is placed lower than the heart
- Local anesthesia of referred tooth/teeth does not eliminate pain while topical anesthesia of nasal mucosa will eliminate the pain if the etiology lies in the nasal mucosa
- Different diagnostic aids used to diagnose sinus disease include paranasal sinus view, computed tomography imaging, and nasal ultrasound
Psychogenic Toothache:
This is a category of mental disorders in which a patient may complain of physical condition without the presence of any physical signs. It must be noted that psychogenic pain is rare. So, all other possible diagnoses must be ruled out before making the diagnosis of psychogenic pain.
The following features are found in psychogenic toothache:
- Pain is observed in multiple teeth
- Precipitated by severe psychological stress
- Frequent changes in character, location, and intensity of pain
- Response to therapy varies which can include a lack of response or an unusual response
- Usually referred to a psychiatrist for further management
Leave a Reply