Ethical And Legal Issues In Clinical Practice
Table of Contents
“…. What is not negotiable is that our profession exists to serve the patient, whose interests come first None but a saint could follow this principle all the time but so many doctors have followed it so much of the time that the profession has been generally held in high regard. — Sir Theodore Fox
Medicine is regarded as a noble profession because physicians are charged with tire supreme responsibility of maintaining health and preserving life of their fellow human beings.
There is an age-old faith, trust, and respect towards physicians in Indian culture. The doctor is often viewed as a demi-god and his advice is usually considered as a gospel truth without any doubt and misgivings.
Read and Learn More Pediatric Clinical Methods Notes
This imposes an onerous responsibility on the part of physicians to be ethical, up-todate, and honest in their approach and dealings with his patients. Physicians are both morally and legally accountable to the society.
The legendary bond of faith between the doctor and patient is best summed up by Charaka: “No other gift is greater than the gift of life! The patient may doubt his relatives, his sons and even his parents, but he has full faith in his physician.
He gives himself up in the doctor’s hands and has no misgivings about him. Therefore, it is the physician’s duty to look after him as his own.”
Due to rapid strides in medical technology over the years, medical care of sick children have unfolded complex medical, social, ethical, philosophical, moral, and legal issues.
It is a sad reality that physicians are allowing technology to dehumanize medicine. The focus of medicine has gradually shifted from the whole patient to his systems, organs, tissues, cells, and even DNA!
Several physicians have fallen into the trap of treating laboratory reports rather than viewing the patient in the wider context of his individuality and social milieu. It is a sad reality that the art of medicine is being sacrificed at the altar of scientific advances and technology boom.
The Consumer Protection Act
‘The people who trust their doctor and surrender themselves to his care are more likely to recover than those who approach medicine with distrust, fear, and antagonism. — Anonymous
Physicians are both morally and legally accountable to society. The doctors are expected to provide efficient and effective medical services to the best of their capabilities in a humane and compassionate manner.
The doctors are liable under the existent criminal laws for acts of negligence. But the legal procedure is time-consirming, expensive, and tedious to get speedy justice.
The medical councils have failed in their responsibility and obligations to serve as watchdogs to identify and penalize medical practitioners indulging in professional misconduct and various malpractices.
In order to rectify this anomaly and ensure speedy compensation to the aggrieved party, the Supreme Court has decreed that the medical practitioners, like other professionals, shall be liable to pay compensation under the purview of 1986
Consumer Protection Act (CPA). When a physician or hospital provides services free of charge to all patients, the CPA cannot be invoked for claiming any damages.
Otherwise, both the acts of negligence as well as the “Deficiency in service” or “substandard services” are covered under the ambit of CPA.
The Supreme Court has conceded to the contention of the Indian Medical Association, that the summary trial of CPA should be limited to only gross or glaring acts of medical negligence.
The complex and technical cases of medical negligence shall be handled, as before, by the civil or criminal courts in accordance with the prescribed procedure and with the help of expert testimony.
In a recent judgment, Supreme Court has opined that doctors cannot be charged as criminals for the death or disability of patients under their care unless there is evidence for a gross and glaring professional neglect.
In order to reduce the menace of criminal proceedings against doctors on frivolous grounds and provide a healing touch to the deteriorating doctor-patient relationship.
The Supreme Court of India has made a historic judgment on February 10th, 2010 which states, “….. It is the bounden duty of civil society to ensure that the medical professionals are not unnecessarily harassed by the complainant who uses the criminal process.
As a tool for pressurizing the medical professionals and hospitals for extracting uncalled-for compensation. It would not be conducive to the efficiency of the medical profession if a doctor is to administer medicine with a halter around his neck”.
Most academic bodies and state medical councils believe that the CPA is unjustified because medical service is neither a commodity nor a contract.
It is impossible to predict the outcome of medical therapy or surgical procedure due to a large number of biological variables because no two human beings are alike.
It is argued that the cost of medical care would escalate because the doctors may indulge in “Defensive medicine” (with unnecessary laboratory tests and diagnostic procedures) and they would also try to recover the costs paid for their indemnity insurance, hi order to avoid litigation, the doctors may refuse to treat critically sick patients or patients with complex medical problems.
The absence of court fee and stamp duty may lead to the filing of frivolous cases. The lack of expert technical advice may adversely affect the process of making rational decisions.
Above all, it is argued that the CPA would erode the doctor-patient relationship of trust and faith which is crucial for the promotion of healing and speedy recovery.
It is indeed a paradox that medical councils have no powers to penalize unqualified medical practitioners or quacks because they do not come even under the purview of CPA!
The consumer activists, on the other hand, strongly believe that the CPA would tame the doctors to improve their accountability and credibility.
They believe that doctors are providing services, like other experts and they ought to have updated medical information and technical competence to handle their patients with confidence and efficiency.
Medicine is already working like a commercial industry and the cost of Medicare is sky rocketing in order to recover the cost of medical education obtained from private medical colleges and the cost of investment in the purchase of high-tech equipment.
It is true that most patients do not suspect the competence and technical expertise of doctors because it is assumed that a qualified doctor is competent. But they do want a doctor who would
listen to them, analyze their medico-psychosocial problems and they should have the option to see the same doctor to establish a relationship of trust and confidence and are assured of continuity of care.
Patients want a competent, caring, and concerned doctor rather than a highly evolved technocrat, hi to a study conducted by the Association of Consumer Action
Safety and Health (CASH), it has been found that lack of proper communication is indeed the most common reason for taking recourse to CPA.
Even in the highly litigous society of the USA, it has been found that most patients sue their doctors because of lack of communication rather than due to lack of expertise and medical knowledge.
The commonest trigger and annoyance on the part of the litigant is always the evasive, unconcerned or insensitive behavior of the doctor, and technical issues are exploited (often with the help of co-professionals) merely to support the allegations and grievances.
Other important reasons for seeking compensation include lack of basic infrastructure, defective or malfunctioning lifesaving medical equipment (Ambu bags, suction equipment, oxygen) and lack of accountability of health care professionals in most government and public sector hospitals.
Common reasons for taking recourse against doctors under CPA:
- Lack of proper communication. Instigation by jealous professional ‘friendsâ€.
- Rude, inconsiderate, unsympathetic, and casual behavior of the doctor.
- Unsatisfactory and unfriendly hospital ethos and lack of facilities.
- Substandard, defective, and malfunctioning medical equipment.
- Unsatisfactory medical record keeping.
- Indiscriminate use of high-tech expensive investigations.
- Lack of clear, and unambiguous expert opinion.
- Lack of knowledge and expertise.
Based on a study conducted by the Association of Consumer Action Safety and Health (ACASH)
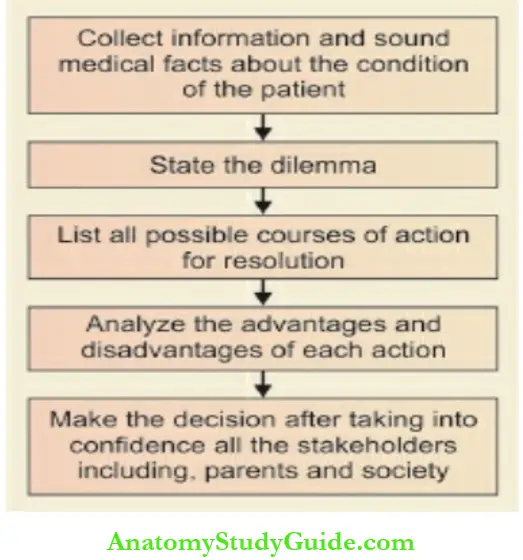
Guidelines for making Ethical Decisions:
Ethical decisions are based on five principles of beneficence, non-maleficence, parental autonomy, correct medical facts, and justice.
Beneficence bequeathed that doctors should be the best advocates of their patients and ensure their best interests in accordance with the age-old
Hippocratic tradition. Physicians should be concerned with saving lives and they should avoid doing any wilful harm to their patients, i.e. there should be non-maleficence in their diagnostic and therapeutic actions.
Florence Nightingale also said that the first dictum of patient care is “Do no harm”. Almost 1000 years ago, according to Manu’s code of conduct for physicians, it was ordained that you should “dedicate yourself entirely to helping the sick, even though this may be at the cost of your own life. Never harm the sick, not even in thoughts.
May the gods help you if you follow this rule. Otherwise, may the gods be against you”. The autonomy and wishes of parents should be honored and they should be taken into confidence while making a decision regarding the medical care of their children through a process of informed consent.
The correct ethical decisions are based on sound medical facts. The principle of justice demands that we seek the morally correct distribution of resources, ensure the cost-effectiveness of therapeutic interventions by balancing medical benefits and burdens to the family and society.
The principle of justice and fairness is often sacrificed in a developing country because due to a lack of resources even essential care and therapy may be denied to indigent patients.
The steps in ethical decision-making are shown in below. A large number of other factors and considerations are taken into account while making a decision in the case of children with life-threatening medical disorders.
Is there a reasonable chance of survival of the child with the available technology or efforts are likely to be futile?
Would the quality of life be worthwhile, if the child survives with aggressive management? Can the family afford expensive intensive care management?
Should we be concerned with the best interests of the child alone or the global interests of the family, society, and state?
Also there are cultural considerations, the fertility of the couple, the concept of destiny or will of God, the doctor knows-the-best attitude, socioeconomic status, education of parents, gender of the child, social support system, and national priorities.
It is unfortunate but true that in a developing country, economic and social realities may out weigh and override ethical considerations.
Obligations Towards Patients:
The professional qualities and attributes of a pediatrician are listed in should provide holistic care to patients under his care with due competence, consideration, and compassion.
Physician is not duty-bound to treat each and every patient asking for his services. But, he has a moral obligation to provide emergency care to his regular patients as and when it is sought.
However, in the absence of a pre-existing relationship, physician is not ethically obliged to provide care to every patient unless no other physician is available in tire nearby vicinity in tire event of a dire emergency.
When a physician finds himself technically incompetent to handle the clinical problem, he should make a referral to an appropriate consultant after discussing with the family.
Patients should be handled in a technically appropriate, transparent and efficient manner without unnecessary laboratory investigations.
Physicians are duty bound to provide competent and humane care to all patients including those with HIV infection. The information obtained during the course of clinical evaluation should be kept as a guarded secret by the physician.
The information should only be released with due consent of the patient or when sought by a court of Law. However, when a patient is suffering from a notifiable disease, physician is duty-bound to bring it to the attention of public health authorities.
The sense of duty towards a patient and society should take precedence over undue concern for monetary compensation or rewards.
Professional qualities, duties, and attributes of a pediatrician:
- Dress smartly, exhibit pleasant demeanor, and greet the child/parent with a smile.
- Be humble, honest, trustworthy, and open, and act with integrity and without any ulterior motive.
- Care of the patient should be our topmost priority.
- Protect and promote the health of our patients and children in the community.
- Be a good listener and establish cordial doctor-patient and doctor-parent relationships.
- Be up-to-date in our knowledge and skills and provide a good standard of evidence-based medicalcare.
- Treat children as children and respect the dignity of our patients and their parents.
- Be humane, compassionate, and responsive to the needs of children and their parents.
- Never make a slighting remark against our professional colleagues.
- We should not allow the technology to further dehumanize medicine and we must treat children not only with our heads but also with our hearts.’
- We must strive to become good human beingbefore we can become good doctor!
Rational Investigations:
There is no denying the fact that a large number of unnecessary investigations are being undertaken because of the lure of “cuts” being offered by the ever-mushrooming diagnostic centers in the country.
It is a sad reality that laboratory investigations have become a substitute for taking a detailed history and conducting a complete physical examination.
At times, excessive and unnecessary investigations are justified as a safeguard against the increasing trend of seeking legal action by consumers.
It is not uncommon to see that most cases of headache are investigated by doing a CT scan of brain but without doing any ophthalmologic and ENT evaluation.
Every case of cerebral palsy is investigated by doing a CT scan and MRI of the brain which has no diagnostic or therapeutic implications.
Some pediatricians are known to monitor the extent of hepato-splenomegaly with the help of serial ultrasound examinations of the abdomen instead of doing a careful physical examination.
In private hospitals, doctors are vying with each other to generate revenue for the hospital by fair or foul means because that is the sole criteria of their survival in the system.
The practice of ordering a routine battery of tests in every patient must be condemned. Instead, the choice of investigations must be individualized in every patient depending upon the diagnostic possibilities based on a detailed clinical evaluation.
It is important that only those investigations should be undertaken which are likely to provide a clue or confirmation to a diagnosis or provide guidelines for rational management of the disease process.
Unethical Practices:
There is increasing commercialization and a gradual decline of human values at all levels of our society. The common correlates and types of unethical medical practices are listed in
It is true that doctors are also human beings but medicine should not be considered merely as another profession but rather a mission in life.
Due to exorbitant cost of medical education in the private sector, upcoming doctors may resort to unethical practices to make quick buck or try to become rich overnight in order to pay back their loans or debt.
Unlike many other professions, the medical profession has a long incubation period of protracted studies (graduate, post-graduate, post-doctoral, clinical experience) before a decent regular job can be bagged or clinical practice is established.
A number of national and international academic bodies and councils have provided moral guidelines and code of conduct for the acceptable and dignified professional conduct of physicians.
The following medical practices are considered as unjustified and unethical
Common correlates and types of unethical medical practices:
- Change of social values and everyone wants to become ‘rich overnight.
- Doctors are competing with each other to createrevenue for the corporate hospital by fair or foulmeans.
- Exhorbitant cost of medical education in the private sector and need to earn fast to pay back the loan.
- Unnecessary diagnostic studies to get ‘cuts’ or the laboratory is owned by the physician. ‘Kickbacks’ for referrals.
- Superfluous medical procedures, like endoscopies and biopsies.
- Needless hospital admissions.
- Unnecessary surgical procedures or even surgical operations.
- Self-promotion through advertisements.
Self-advertisement, glorification, display of large signboards, self-aggrandizement, and claim of miracle therapies in lay press are unethical practices.
A medical practitioner is permitted to make a formal announcement in press regarding the start of private practice, intimate the change of address, temporary nonavailability and resumption of practice for tire information of his clients.
Physicians can charge a reasonable professional fee depending upon their seniority and expertise but should not indulge in unfair practices, like receiving “cuts” from their specialist colleagues for referring patients to them.
Due to mushrooming of diagnostic facilities and cut throat competition, many laboratories are enticing tire physicians by offering “Kick-backs” to them to refer patients for investigations.
It is a sad reality, that in order to make quick money, many unnecessary or irrelevant investigations are ordered and they are justified or legitimized in tire garb of a safeguard against tire viles and vagaries of the Consumer Protection Act.
The practice of ordering a battery of tests merely to receive gratification or “Cuts” from tire laboratory is unethical and is strongly condemned.
Unnecessary admissions of patients to tire hospital for treatment or undertaking a diagnostic or surgical procedure that is unwarranted is unethical.
During our clinical practice, we screen a large number of prescriptions and investigations conducted by our colleagues.
We must review them without arrogance and with due humility without making any adverse remarks or showing it through our body language.
We must treat our doctor colleagues as members of a big family and we should never utter a disparaging word or remark against our professional colleagues. Sir William Osier has extolled that
“Never let your tongue say a slighting word of a colleague”. Medicine should be practiced with conscience and dignity and without any greed of motive or profit.
It is unethical and illegal to abet “Female foeticide” by prenatal determination of sex by ultrasonography. Nothing should be done in our day-to-day dealings and practice which hurts our inner voice or conscience in order to prevent guilt feelings and remorse.
It is unethical to take any overt or covert sexual liberties or exhibit misconduct with patients or their attendants whether in thought, behavior, or action.
It is unethical and fraudulent to issue false medical certificates or disability certificates for financial considerations. The physician should provide true information with a sense of fairness, honesty, and integrity.
The public and patients should not be blackmailed or put into inconvenience by striking work or adopting work-to-rule mandates by doctors in government institutions to get their demands fulfilled under duress.
Instead of harassing the patients, they should harness the support of the public to get their just demands fulfilled.
The government of India has brought medical services under the ambit of. Essential Service Maintenance Act (ESMA) to put a curb against the menace of strikes by doctors.
It is unethical, illegal, and immoral to trade the body organs for transplantation for pecuniar or financial considerations.
It is unscrupulous and dishonest for physicians to receive courtesies, favors and gifts from manufacturers and suppliers of equipment and pharmaceutical companies.
The Medical Council of India has recently issued guidelines and directives to promote ethical relationship between doctors and companies producing health care products
Research must be conducted with fairness, sincerity, and with due safeguards to the study subjects.
The medical profession should ensure the safety and efficacy of new technologies and informed consent must be taken before recruiting patients for therapeutic interventions and drug trials.
Fraud in research either by plagiarization or “Quantum jugglery” are condemned and punished for professional misconduct. The researcher should not misrepresent the ideas of others as his own.
Medical Council of India’s directives to promote ethical practices:
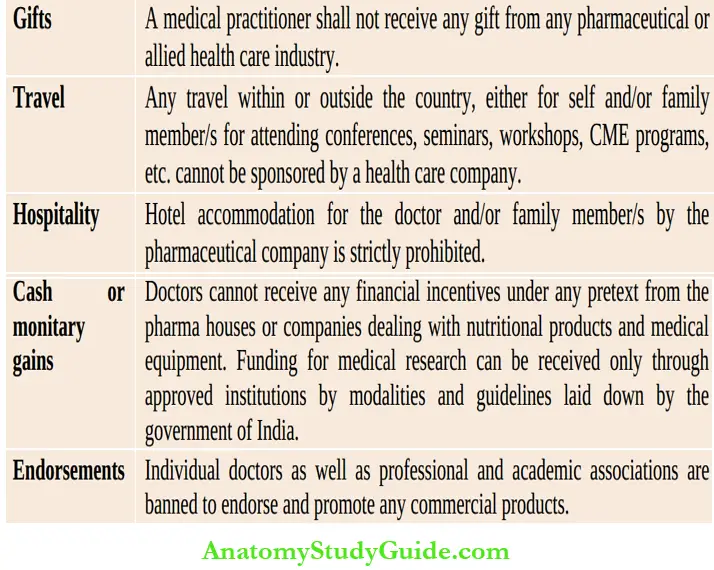
The violation of any of the MCI directives shall be considered as “Misconduct” and, therefore, can invite penalties in the form of temporary or protracted suspension or cancellation of registration to do the medical practice.
However, the implementation of these guidelines is a major challenge for the Medical Council of India.
Withholding or Withdrawal of Life Support:
Cardiopulmonary resuscitation is withheld, if a patient is terminally sick or it is believed that the available therapies are likely to be futile and in the event of survival there will be virtual or total loss of cognition for any meaningful existence.
Humanistic teachings in general and philosophies of the major religions of the world recognize that there comes a time in the care of every patient when it is appropriate for the doctor to stop further attempts to prolong unnecessarily the process of dying.
The policy of passive euthanasia is followed by withholding CPR, life-saving surgery, assisted ventilation, dialysis, vasopressors, administration of blood and blood products, and expensive antibiotics.
Instead of a continuation of life-prolonging therapy, it is desirable to provide palliative care to relieve pain and suffering.
Indications for do-not-resuscitate (DNR) orders:
- Advanced metastatic malignancy
- Multisystem end-stage organ failure
- Severe irreversible CNS disorder, trauma, bleeding, and tumor
- Severe and untreatable underlying neuromotor disability
- Persistent vegetative state
- Braindead
This is an indication for withdrawal from life support
The decision to withhold or withdraw life support should be taken after due deliberations among various experts by taking the family into confidence through the process of informed consent.
The decision should be recorded in the case file along with full medical justifications and should be duly signed by the parent or surrogate.
This approach is duly approved by the professional and academic bodies of the world. The policy is logical and rational and is aimed at reducing the suffering and misery of both the dying patient and his close relatives.
But it lacks legal sanction and protection. There is a need to accord legal sanctity to the act of passive euthanasia in order to avoid unnecessary litigations.
Tin procedure manual in the PICU should outline details of admission policies, indication! for withdrawal, and withholding of life support.
Communication and Doctor-patient Relationship:
‘A person may have learned a great deal and still be an exceedingly unskillful physician, who awakens little confidence in his powers … The manner of dealing with patients, art of winning their confidence, soothing and consoling them, or drawing their attention to serious matters … all this cannot be learned from books. —John Apley
Most parental complaints of mismanagement originate due to lack of conmumication or because of abrasive, cold or callous attitude of the doctor or health team rather than due to lack of skills or faulty technical management of the patient.
Don’t judge, be little or argue with parents. Humility, concern, empathy and compassion are crucial to generate faith and provide emotional support to the family.
Even if the enquiry or query of the parents is illogical, repetitive and irritating, we must respond with due grace, sensitivity, equanimity and calmness without any hurry, anger or arrogance.
Communication is indeed the most vital link to strengthen doctorpatient relationship. Tire virtues and benefits of good doctor-patient communication are listed in
Benefits of good doctor-patient/parent communication:
- Better confidence, trust, and faith in the physician.
- Reduced anxiety and greater satisfaction of the patients and parents.
- Provision of holistic care rather than mere cure.
- Better compliance to therapeutic options.
- Better health outcomes.
- Reduced risk of malpractice litigations.
It is an amazing fact that most parents are grateful even when we are unable to save the life of their child especially if one showed concern, care, and compassion and parents and relatives were made to perceive that whatever was humanely possible was done for the care of their child.
It is important to communicate “with” parents by literally coming down to their level and by maintaining eye-to-eye contact.
We should be careful and tactful not only in deciding “What to tell” the parents but also “How to tell it”. The parents should be told about the condition of the child in a simple, easily understandable language.
We should try to be pragmatic and honest in communicating the true status of the child but nevertheless try to keep the hope alive which has tremendous healing capabilities, hi a critically sick child, always give a guarded prognosis which can be tempered with hope, will power and godly benevolence.
Chronic or Incurable Disease:
When a child is suffering from an incurable disease or an affliction that is likely to have lifelong disability, the parents are likely to respond with disbelief, anger, shock or feeling of hopelessness.
The bad news should preferably be conveyed to both parents simultaneously in a relaxed atmosphere with due concern, compassion, and empathy.
The facts should be explained in a simple language without any medical jargon.
The nature of disease, likely prognosis, available therapeutic interventions and cost of care, etc. should be explained. We should allow the parents to ventilate their feelings and concerns and try to answer their queries in an honest and unambiguous maimer.
We should try to follow the well-known philosophy, “Talk less and listen more”, that is why God has given us one mouth and two ears! We should be pragmatic but not pessimistic and always keep the hope alive which is a great healing force and remember that miracles do happen.
We should be careful and diplomatic in conveying the nature of the disease without hurting parental sentiments. Instead of saying bluntly that “your child is mentally retarded”, it is preferable to say that your child is slow or having a developmental delay.
In our society, it is important to provide spiritual dimension to their tragedy by saying that “God has chosen you to provide care and comfort to your special child because you are so compassionate, caring, and sensitive human being”.
The family should be encouraged to join the Self-Help Association of Parents of children having the same medical problem to form a network and learn from each other by sharing mutual concerns and difficulties and by effective utilization of available technologies and specialist services.
The End-of-life Issues:
“Death is certain for the born and rebirth is inevitable for the dead. You should not, therefore, grieve over the inevitable”. —The Bhagavad Cita
Despite all the technological advances, medicine cannot achieve immortality. We are all destined to die and death indeed is the ultimate truth of life.
But death is always unacceptable especially when life is cut short in the bud without fulfillment of purpose of existence or when it is due to unnatural causes.
It is easier to face death when it is anticipated and family is adequately prepared for the eventuality.
Pediatricians face several situations in clinical practice wherein a child is diagnosed to have a potentially fatal disease (AIDS, malignancy, genetic disorder) or develops an acute lifethreatening disorder or dies suddenly in the emergency room due to polytrauma or road accident.
The news of an incurable or difficult-to-manage intractable disease should be given to both the parents in a relaxed manner with due consideration and compassion.
Parents must be given an opportunity to ask questions and vent their feelings and you must listen attentively and provide appropriate answers to relieve their anxiety, concerns and worries.
It is controversial as to how much information should be given to the child and whether he or she should be taken into confidence and told about the nature of the disease or it should be kept as a guarded secret.
By and large, it depends upon the age, inquisitiveness, sensitivity and emotional maturity of the child whether he should be told about the nature of disease or not but you must seek the advice of parents in this matter.
The news about the “Bad” disease should never be conveyed bluntly like a bolt from the blue. You should be honest and pragmatic in your approach and the news of “Gloomy prognosis” must be tempered with due optimism and godly benevolence to keep the hope alive in order to augment the process of healing.
We do know that nature, time, patience, faith, hope, prayer, positive thinking and willpower have tremendous healing capabilities and they should be effectively harnessed in our day-to-day clinical practice.
The family should be prepared emotionally and spiritually before declaration of death. The news of death should be conveyed with utmost compassion but in no immistakable term that the child has died despite our best intentions and efforts.
Acceptance of death becomes difficult when a child dies in the Emergency Department due to an acute life-threatening disease or road accident.
A large number of emotions, like anger, hostility, shock, grief, guilt, denial, and depression, need to be handled with poise, sympathy and utmost care so that reality is accepted with due grace as a will of God or nature’s ordain and as a matter of fact or destiny.
If CPR is being provided (where DNR is not applicable), the parent or attendant should be escorted to the restroom and allowed to vent his/her feelings.
The family’s wishes for religious support (amulets, mantras, holy water, etc.) and ceremonies and their desire that the death should occur in the familiar atmosphere of home rather than a hospital, should be honored as far as possible.
When a child is conscious and dying, the parents should be at his bedside holding Iris hand and talking with him to allay his fears and assist him to express his concerns, desires, and emotions.
Silent listening and support at tins stage is valued more than unnecessary talking.
During the emotionally surcharged atmosphere of the process of dying, some resident doctors and nurses may feel extremely frustrated, upset, and demoralized because of their inadequacy and inability to save life despite sincere and maximal efforts.
They also need emotional support, guidance, and advice to avoid unnecessary identification and attachment with the family. They should be encouraged and assisted to learn the art of detachment, imperturbability, and poise at all odds.
After taking relevant postmortem biopsies, the family should be approached with caution and tact to seek permission for an autopsy.
You should never give the impression that an autopsy is needed for making a correct diagnosis but it is required for helping science and society regarding the prevention of disease among contacts and siblings and for possible genetic coimseling.
After completing urgent formalities, a death certificate should be prepared. The family should be provided with the necessary courtesy, compassion, and conveyance for a dignified journey of the dead child to the mortuary or home.
The coping of the death of a child in the hospital is a painful and challenging experience but one that can also provide respect for humanity and life.
Death deflates our ego and teaches us humility and provides strength to face and accept the greatest reality and truth of life with equanimity and grace.
Organ Transplantation:
The enaction of the Human Organ Transplant Act by the Indian Parliament in 1994 has opened opportunities for cadaveric transplants of the heart, liver, kidneys, pancreas, etc., which should be fully exploited.
The possibility of a positive contribution through their tragedy with the hope that their child may see the world or live through somebody else’s eyes or organs may be accepted with enthusiasm.
The issue of organ donation should not be broached, if there are well recognized contraindications for a donation of organs, such as primary immunodeficiency disorder, genetic defect, HIV, HBs Ag-positivity, viremia, and septicemia.
Xenotransplantation (animal-to-human transplant) of cells, tissues and organs with or without genetic engineering is fraught with serious hazards of transmission of animal viruses, rejection, social injustice, and moral and religious considerations.
Conclusions:
The declining image of the medical profession needs a moral boost and rejuvenation through a process of soul searching and ethical cleansing in the light of existent social realities.
The continuing process of erosion of doctor-patient relationships and trust due to the insensitive and commercialized attitude of some physicians and over demanding attitude of educated and well-informed internet-savvy parents needs to be checked against further disintegration.
In view of the fact that services of the doctors have been included in the purview of Consumer Protection.
Act for redressal of grievances and grant of compensation by the consumer courts, it is essential for the doctors to be more cautious, considerate and ethical in their dealings with their patients to avoid any unnecessary litigations.
The revolution in technology is no substitute for undermining the need for trust and communication which indeed is the key to maintaining an ideal doctor-patient
relationship.
It is desirable that all medical colleges in the country should initiate regular education programs in the field of social and behavioral sciences, the art of communication, and medical ethics for graduate and postgraduate medical and nursing students.
The teachers must serve as role models to infuse and enthuse the qualities of compassion, sensitivity, and genuine concern toward patients and their attendants.
We should not allow technology to further dehumanize medicine and we must treat children not only with our heads but also with our hearts.
The world needs caring and concerned physicians, and not merely curing and commercial robots who lack sensitivity and deny the healing virtues of the human touch.
Ethics and grievances committees should be established in all hospitals and they should serve as watchdogs to monitor and maintain the sanctity of all ethical decisions.
It is nice to have up-to-date knowledge and be a well-formed doctor but above all it is much nicer to be a good human being in order to provide global and holistic care rather than mere cure to one’s patients.
Physicians should make concerted efforts to resurrect the medical image, master the sublime art of medicine and acquire the divine gift of healing.
Leave a Reply