Female Genital Tract
Question 1. Write a short note on the embryonal rhabdomyosarcoma of the vagina.
Answer:
Embryonal rhabdomyosarcoma
- Also called sarcoma botryoides
- Age group: Infants and children younger than 5 years of age
- The tumor grows as polypoidal, rounded, bulky masses
- Appears as grape-like clusters (hence the designation botryoid, or grape-like)
Read and Learn More Preparatory Manual of Pathology Question and Answers
Microscopy
- Composed of tumor cells containing undifferentiated round or spindle cells in a myxoid stroma
- The cytoplasm of tumor cells can show striations (indicative of muscle differentiation)
- A characteristic feature is the presence of the ‘cambium layer’ which is a distinctive subepithelial dense zone and separates tumor cells from the squamous epithelium
Question 2. Write a short note on cervical intraepithelial neoplasia (CIN).
Answer:
Cervical intraepithelial neoplasia (squamous intraepithelial lesions):
Classification systems for squamous cervical precursor lesions:
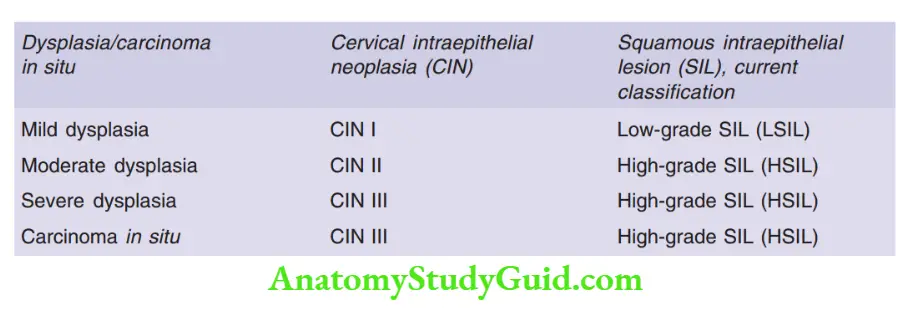
Morphology
Squamous intraepithelial lesion (SIL)
- Characterized by nuclear enlargement, hyperchromasia, coarse chromatin, and variation in nuclear size and shape
Grading of SIL
- LSIL (CIN I) is characterized by pilocytic atypia (nuclear alterations with a perinuclear halo) and involves lower than one-third of the epithelial thickness
- HSIL (CIN II) is characterized by progressive atypia and expansion of immature basal cells above the lower third of the epithelial thickness
- HSIL (CIN III) is characterized by diffuse atypia, loss of maturation, and expansion of the immature basal cells to the epithelial surface, full-thickness dysplasia
Question 3. A 40-year female presents with post-coital bleeding and foul-smelling discharge per vagina. She also complained of a loss of 15% body weight in the past 2 months, accompanied by a loss of appetite.
1. What is your diagnosis?
2. What etiopathogenesis of this condition?
3. What are the morphological features?
4. Write the staging of the disease, which patient is suffering from?
Answer:
1 . Diagnosis is squamous cell carcinoma of the cervix
2 . Pathogenesis of squamous cell carcinoma cervix:
- High-risk HPVs (most commonly HPV-16 and 18) are the most important factors in the development of cervical cancer
- HPVs infect immature basal cells of the squamous epithelium, in areas of epithelial breaks, or immature metaplastic squamous cells present at the squamocolumnar junction
- HPVs replicate in mature squamous cells
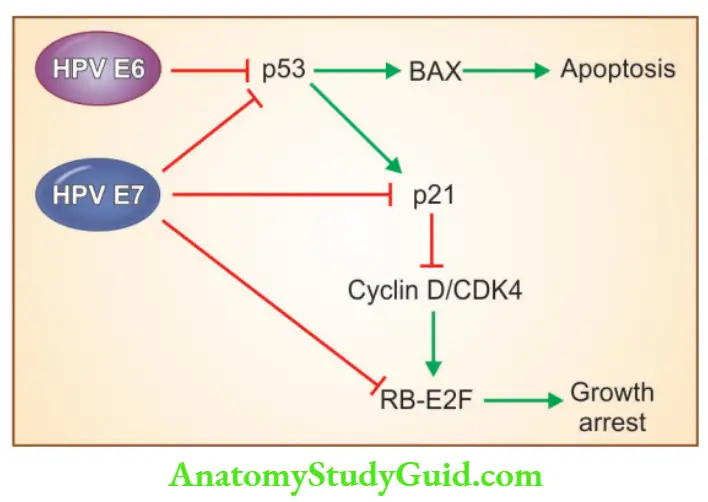
- HPV is carcinogenic due to its viral proteins E6 and E7
HPV E6 protein:
- This leads to degradation of p53, which results in uncontrolled stimulation of cyclin/ cyclin-dependent kinases and thus increased cell cycle proliferation
- Stimulates the expression of TERT, the catalytic subunit of telomerase, and inhibits cell death
HPV E7 protein:
- Binds to the RB protein and displaces the E2F transcription factors that are normally sequestered by RB, promoting the progression of the cell cycle
- Inactivates the CDK inhibitors p21 and p27, which result in uncontrolled stimulation of cyclin/cyclin-dependent kinases and thus increased cell cycle proliferation
3. Morphology
Gross
- Can present either as fungating (exophytic) or infiltrative masses
Microscopy
- Squamous cell carcinoma is composed of nests of malignant squamous epithelium (keratinizing or non-keratinizing) which invades the underlying cervical stroma
Staging of cervical cancer
Stage 0: Carcinoma in situ (CIN III, HSIL)
Stage I: Carcinoma confined to the cervix
- Ia: Preclinical carcinoma (diagnosed only by microscopy)
- Ia1: Stromal invasion, no deeper than 3 mm and no wider than 7 mm (so-called micro-invasive carcinoma)
- Ia2: Maximum depth of invasion of stroma deeper than 3 mm; horizontal invasion not more than 7 mm
- Ib: Histologically invasive carcinoma confined to the cervix and greater than stage Ia2
Stage II: Carcinoma extends beyond the cervix but not to the pelvic wall. Carcinoma involves the vagina but not the lower third
Stage III: Carcinoma has extended to the pelvic wall. On rectal examination, there is no cancer-free space between the tumor and the pelvic wall. The tumor involves the lower third of the vagina
Stage IV: Carcinoma has extended beyond the true pelvis or has involved the mucosa of the bladder or rectum. This stage also includes cancers with metastatic dissemination
Question 4. Write a short note on endometriosis.
Answer:
Endometriosis
- Definition: Presence of “ectopic” endometrial tissue at a site outside the uterus
- Abnormal tissue includes both endometrial glands and stroma
- Sites: Ovaries, uterine ligaments, rectovaginal septum, cul-de-sac
- Clinical features: Infertility, dysmenorrhea (painful menstruation), pelvic pain, dyspareunia (pain while intercourse)
Pathogenesis
1. Regurgitation theory
- Endometrial tissue implants at ectopic sites via a retrograde flow of menstrual endometrium
2. Benign metastases theory
- Endometrial tissue from the uterus can “spread” to distant sites (for example bone, lung, and brain) via blood vessels and lymphatic channels
3. Extra-uterine stem/progenitor cell theory
- Stem/progenitor cells from the bone marrow differentiate into endometrial tissue
Morphology
- Presents as red-blue to yellow-brown nodules on mucosal and/or serosal surfaces
- Ovaries (chocolate cysts or endometriomas) are distorted by large cystic masses (3 to 5 cm in diameter) which are filled with brown fluid resulting from previous hemorrhage
- Histological diagnosis is made when both endometrial glands and stroma are present in the biopsy studied
Question 5. Write a short note on adenomyosis.
Answer:
Adenomyosis
- Definition: Presence of endometrial tissue within the uterine wall (myometrium)
- Microscopy: Irregular nests of endometrial stroma, with or without glands, are present within the myometrium, separated from the basalis layer by at least 2 to 3 mm
- Clinical features: Menometrorrhagia (irregular and heavy menses), colicky dysmenorrhea, dyspareunia, and pelvic pain
Question 6. Classify endometrial carcinomas. Write a note about a malignant mixed müllerian tumor.
Answer:
Carcinoma of endometrium
Type I (endometrial) carcinoma
- Most common type
- Well-differentiated type
- Mimic proliferative endometrial glands
- Referred to as endometrioid carcinoma
- Arises in the setting of endometrial hyperplasia
- Associated with: Unopposed estrogen, obesity, hypertension, diabetes
Type II (serous) carcinoma
- Includes serous carcinoma (most common), clear cell carcinoma, and malignant mixed müllerian tumor
- Occurs in older women
- Arises in the setting of endometrial atrophy
- Poorly differentiated (grade 3) tumors
Malignant mixed müllerian tumors (MMMTs)
- Also called carcinosarcomas
- Endometrial adenocarcinoma with a malignant mesenchymal component
Morphology
- Gross: Tumors are bulky and polypoidal, which protrude through the cervical os
- Microscopy: Tumors usually consist of adenocarcinoma (endometrioid, serous or clear cell) mixed with the malignant mesenchymal (sarcomatous) elements
- Sarcomatous components may include striated muscle, cartilage, adipose tissue, and bone
- Metastases contain only epithelial components
Question 7. Write a short note on Leiomyoma uteri.
Answer:
Leiomyoma
- Uterine leiomyoma (fibroid) is the most common tumor in women
- Benign smooth muscle neoplasm which may occur singly, or often multiple
Chromosomal abnormality
- Rearrangements of chromosomes 12q14 and 6p involving the HMGIC and HMGIY genes respectively are seen
- Mutations in the MED12 gene are common
Morphology
Gross
- Sharply circumscribed, discrete, round, firm, gray-white tumors varying in size from small nodules to massive tumors
- Fibroids can be: Intramural (within the myometrium), u-mucosal (just beneath the endometrium), or sub-serosal (beneath the serosa)
Cut surface
- The characteristic whorled pattern of smooth muscle bundles
Microscopy
- Leiomyomas are composed of bundles of smooth muscle cells
- Individual muscle cells have characteristic oval nuclei and long, slender bipolar cytoplasmic processes
Variants:
- Atypical or bizarre tumors with nuclear atypia and giant cells
- Cellular leiomyomas
Clinical features
- Abnormal bleeding, increased urinary frequency (due to compression of the bladder), sudden pain from infarction of a large or pedunculated tumor, and impaired fertility
- Myomas in pregnant women increase the frequency of spontaneous abortion, fetal mal-presentation, uterine inertia (failure to contract with sufficient force), and postpartum hemorrhage
Question 8. Classify ovarian neoplasms. Discuss in detail the molecular pathogenesis and morphology of serous tumors.
Answer:
WHO classification of ovarian neoplasms
1. Surface epithelial-stromal tumors
1. Serous tumors
- Benign, borderline, malignant
2. Mucinous tumors, endocervical-like and intestinal type
- Benign, borderline, malignant
3. Endometrioid tumors
- Benign, borderline, malignant (endometrioid adenocarcinoma)
4. Clear cell tumors
- Benign, borderline, malignant
5. Transitional cell tumors
- Benign Brenner tumor, Brenner tumor of borderline malignancy, malignant Brenner tumor
6. Epithelial-stromal
- Adenosarcoma, malignant mixed müllerian tumor
2. Sex cord-stromal tumors
Granulosa cell tumors, fibromas, fibrosarcomas, thecomas, Sertoli-Leydig cell tumors, steroid (lipid) cell tumors
3. Germ cell tumors
- Teratoma immature, mature {solid, cystic (dermoid cyst)}, mono dermal (example struma over, carcinoid)
- Dysgerminoma
- Yolk sac tumor (endodermal sinus tumor)
- Mixed germ cell tumors
4. Metastatic cancer from a non-ovarian primary
- Colonic, appendiceal, gastric, pancreaticobiliary, breast
Etiopathogenesis of serous epithelial tumors
- Age group: 20–45 years (benign and borderline), old age (carcinomas)
- Risk factors for serous carcinomas: Nulliparity, family history, and heritable mutations
- Oral contraceptives and tubal ligation reduce the risk
- BRCA-1 and BRCA-2 increase susceptibility to ovarian cancer and predispose to high-grade serous carcinomas
Associations of serous carcinomas
- Serous tubal intraepithelial carcinoma (STIC): Occurs in association with high-grade serous ovarian cancers
- Serous ovarian carcinomas arise from cortical inclusion cysts Morphology of serous epithelial tumors
1. Benign tumors
- Gross: Ovary shows a smooth glistening cyst wall with small papillary projections
- Microscopy: Tumor shows stromal papillae, lined by columnar epithelium
2. Borderline tumors
- Gross: Ovary is replaced by a cystic cavity, lined by delicate papillary tumor mass
- Microscopy: Tumor cells arranged in papillae with increased architectural complexity and epithelial cell stratification with mild nuclear atypia
3. Malignant tumors
- Gross: Ovary shows larger areas of solid or papillary tumor mass
- Microscopy: Tumor cell invasion into the adjacent stroma is seen
Question 9. Discuss morphological features of mucinous tumors of the ovary.
Answer:
Mucinous tumors
- Comprises 2–25% of all ovarian neoplasms
- Most commonly benign and borderline tumors
Pathogenesis
- Mutation of the KRAS proto-oncogene is commonly seen in Morphology
- 5% of primary mucinous cystadenomas and mucinous carcinomas are bilateral
Gross
- Appears as multi-loculated cystic masses, with the cysts being filled with gelatinous fluid (can weigh>25 kg)
Microscopy
Classified into 2 types:
1. Intestinal type: Characterized by a papillary architecture lined by tall non-ciliated cells with basal nuclei and abundant intracellular mucin
2. Endocervical type: Characterized by epithelial lining with a ‘picket-fence’ appearance (columnar cells lining the cysts)
Borderline mucinous tumors
- The atypical epithelium is less than four cells in thickness (>4 cell thickness is carcinoma)
Malignant mucinous tumor
- Characterized by cell atypia, increased cell thickness, greater complexity of the glands and papillae (budding, bridging, the appearance of solid foci), with areas of stromal invasion
Question 10. Write a note on the pseudonym Peritonei.
Answer:
Pseudomyxoma peritonei
- Mucinous tumors involving the ovary
- Characterized by extensive deposits of intra-abdominal mucin
- Previously, the pseudonym peritoneal was thought to be due to the spread of mucinous ovarian neoplasm
- But recently it has been shown that it occurs due to metastasis in the ovary from the appendix (most commonly)
Note:
- Mucinous ovarian tumors are mostly unilateral
- Hence, in bilateral ovarian tumors, metastatic ovarian carcinoma has to be ruled out
Question 11. Write a note on Brenner’s tumor.
Answer:
Transitional cell tumor (Brenner tumor)
- Contains neoplastic epithelial cells resembling the urothelium and are mostly benign
Gross
- Solid or cystic
- 90% are unilateral
- Can range in diameter from 1 cm to 20 to 30 cm
Microscopy
- The ovarian stroma contains sharply demarcated nests of epithelial cells resembling the epithelium of the urinary tract
Question 12. Discuss in detail the morphology of the dermoid cyst of the ovary. Mention the components of the struma ovary.
Answer:
Teratomas
1. Mature (benign) teratomas
- Are cystic, so-called dermoid cysts (lined by skin-like structures)
- Seen in the reproductive age group women
Morphology
- Bilateral in 10–15% of cases
Gross
- Unilocular cysts containing hair and sebaceous material
- In the wall, teeth-like structures and areas of calcification are commonly seen
Microscopy
- Derivatives of all three germ cell layers are seen
- The Cyst wall is composed of stratified squamous epithelium with underlying sebaceous glands, hairshafts, and other skin adnexal structures
- Cartilage, bone, thyroid, and neural tissue are commonly seen
- Malignant transformation, most commonly to squamous cell carcinoma or thyroid carcinoma, melanoma can occur
Struma ovarii
- Monodermal or specialized teratomas
- Ovarian stroma is composed of mature thyroid tissue
Question 13. Discuss dysgerminoma of the ovary.
Answer:
Dysgerminoma
- Malignant tumor
- The ovarian counterpart of testicular seminoma
- Occurs in the second and third decades
- Elevated HCG levels can be seen (due to syncytiotrophoblastic giant cells)
- Express OCT-3, OCT4, and NANOG
- Activating mutations in the KIT gene are seen
Morphology
- Unilateral tumors
- Cut surface: Multinodular, solid yellow-white, soft and fleshy
Microscopy
- Tumor cells grow in sheets or cords separated by scant fibrous stroma, which is infiltrated by mature lymphocytes
- Tumor cells are large vesicular, with clear cytoplasm, well-defined cell boundaries, and centrally placed regular nuclei
Question 14. Write a note on the endodermal sinus tumor.
Answer:
Yolk sac tumor (endodermal sinus tumor)
- Neoplasm of Children and young adults
- Tumor cells elaborate α-fetoprotein
Gross
- Tumors can measure up to 15 cm in diameter
- The outer surface is smooth and glistening
- Cut surface: Variegated (heterogeneous), composed of cystic areas admixed with areas of hemorrhage and necrosis
Microscopy
- A glomerulus-like structure composed of a central blood vessel enveloped by tumor cells within a space that is also lined by tumor cells (Schiller-Duval body)
- Intracellular and extracellular hyaline droplets are present
Question 15. Write important features of sex cord-stromal tumors.
Answer:
Sex cord-stromal tumors
- Tumors are derived from the ovarian stroma (which is derived from the sex cords of embryonic gonads)
- Gonadal mesenchyme produces Sertoli cells and Leydig cells in males and granulosa cells and theca cells in females
- As Leydig cells secrete androgens, their corresponding tumors produce masculinizing symptoms
- As granulosa and theca cells secrete estrogens, their corresponding tumors produce feminizing symptoms
Clinical features of Sertoli-Leydig cell tumors
- Defeminization: Atrophy of the breasts, amenorrhea, sterility, and loss of hair
- Masculinization: Virilization (hirsutism) with the male distribution of hair, hypertrophy of the clitoris, and voice change
Question 16. Discuss in detail about granulosa cell tumor of the ovary
Answer:
Granulosa cell tumors
- Resembles granulosa cells of developing ovarian follicle
- Two types: Adult and juvenile granulosa cell tumors
- Most commonly seen in postmenopausal women
Morphology
Gross
- Unilateral, large, solid, cystic encapsulated mass
- Cut surface: Appears yellow due to intracellular lipids
Microscopy
- Tumor cells grow in anastomosing cords, sheets, or nests
- Tumor cells are small, cuboidal to polygonal
- Call-Exner bodies: Small, distinctive, gland-like structures filled with an acidophilic material
Clinical features
- Elaborate large amounts of estrogen
- Are potentially malignant
- Juvenile granulosa cell tumors in pre-pubertal girls may lead to precocious sexual development
- In adults, they may be associated with proliferative breast disease, endometrial hyperplasia, and endometrial carcinoma
- Elevated tissue and serum levels of inhibin (a product of granulosa cells) are seen
- FOXL2 positivity is seen in adult granulosa cell tumors, but it is negative in juvenile granulosa cell tumor
Question 17. Mention briefly about Krukenberg tumor.
Answer:
Krukenberg tumor
- Metastatic gastric carcinoma involving bilateral ovaries
- Microscopy: Metastases composed of mucin-producing, signet ring cancer cells
Question 18. Write a note on the hydatidiform mole.
Answer:
Hydatidiform mole
- Associated with an increased risk of persistent trophoblastic disease (invasive mole) or choriocarcinoma
- Two types complete and partial
1. Complete mole
- Results from fertilization of an ovum that has lost its female chromosomes
- Genetic material is paternally derived
- Androgenesis: 90% have 46, XX karyotype due to the duplication of the genetic material of one sperm
- 10% result from the fertilization of an empty egg by two sperms; these may have 46, XX or 46, XY karyotype
- Fetal parts are not identified as the embryo dies early
- Increased risk for choriocarcinoma and persistent or invasive mole
Gross
- Delicate friable mass of cystic, grape-like structures, which are villi showing hydropic degeneration
Microscopy
- Chorionic villi are enlarged, scalloped in shape with central cavitation (cisterns)
- Circumferential trophoblastic proliferation around the individual villi
2. Partial mole
- Occurs as a result of fertilization of an egg with two sperms
- In these moles, the karyotype is triploid (example 69, XXY)
- Fetal tissues are typically present
- Partial moles have an increased risk of persistent molar disease
- Not associated with increased risk of choriocarcinoma
Microscopy
- The fraction of villi is enlarged and edematous
- Focal trophoblastic hyperplasia
- Villi have an irregular, scalloped outline and contain vessels with fetal (nucleated) red blood cells
Question 19. Describe in detail choriocarcinoma.
Answer:
Choriocarcinoma
- Malignant neoplasm of trophoblastic cells derived from previously normal or abnormal pregnancy (extra-uterine ectopic)
- Rapidly invasive and metastasizes widely
- 50% arise in complete hydatidiform moles, 25% in previous abortions, 22% follow normal pregnancies, and the remaining in ectopic pregnancies
Morphology
- Gross: Soft, fleshy, yellow-white tumor with large areas of necrosis and extensive hemorrhage
Microscopy
- A tumor is composed of clusters of cytotrophoblasts and syncytiotrophoblasts
- Hemorrhage and necrosis are usually present
- Villi are characteristically absent
- Tumor invades the underlying myometrium, penetrates blood vessels, and can extend out onto the uterine serosa and into the adjacent structures
Clinical Features
- Manifests as irregular vaginal spotting of a bloody, brown fluid
- Hematogenous spread is common
- Widespread metastases are characteristic
- The most common sites of metastasis include the lungs, and vagina, followed by the brain, liver, bone, and kidney
- HCG levels are elevated and the levels are above those seen in hydatidiform moles
- Treatment: Evacuation of the contents of the uterus followed by chemotherapy
Question 20. Write a note on sites of ectopic gestation.
Answer:
Ectopic gestation
- Refers to implantation of the fetus at a site other than the normal intrauterine location
- The most common site is the extrauterine fallopian tube (90% of cases)
- Other sites include the ovary, abdominal cavity, and the intrauterine portion of the fallopian tube (cornua pregnancy)
- Causes of ectopic gestation: Pelvic inflammatory disease, peritubular scarring, and adhesions, intrauterine contraceptive device usage
Note: Rupture of tubal pregnancy is a medical emergency
Leave a Reply