Female ♀ Reproductive Organs
Prolapse Of Uterus
1. Definition: Falling down of the uterus or sinking of uterus is called prolapse of the uterus.
Table of Contents
2. Types of prolapse: Prolapse of the uterus with prolapse of
- The urinary bladder is called cystocoele.
- Urethra is called ureterocele.
- Rectum is called rectocele.
- Procidentia: Falling down the cervix through vagina is called procidentia.
Read And Learn More: General Histology Question And Answers
Prolapse Of Uterus
1. Definition: It is downward displacement of uterus from the normal position.
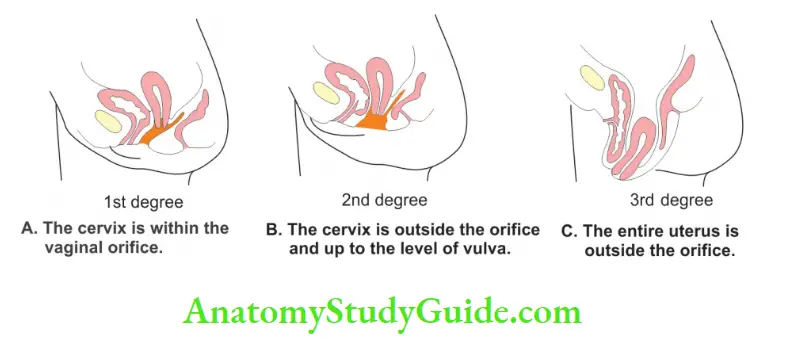
2. Degree of prolapse: Depending upon the extent of displacement of uterus, it is described as
- First degree: The cervix is within the vaginal orifice.
- Second degree: The cervix is outside the orifice and up to the level of vulva.
- Third degree: The entire uterus is outside the orifice.
- Procidentia: The whole uterus is outside the vaginal orifice.
3. Prolapse Of Uterus Causes:
Injury to the perineal body: Is one of the commonest causes of prolapse of uterus. The situation is exacerbated in the presence of a
- Disrupted perineal body or with
- Atrophic pelvic floor.
Predisposing factors:
- Retroversion uterus
- Loss of tone of the muscles of pelvic diaphragm
- Perineal tears, and
- Repeated childbirth
4. Types of prolapse: Prolapse of uterus with prolapse of
- The urinary bladder is called cystocele.
- Urethra is called ureterocele.
- Rectum is called rectocele.
- Procidentia: Falling down the cervix through vagina is called procidentia.
Question – 1: Describe ovary under following heads
1. Gross Anatomy
2. Histology
3. Development, and
4. Applied Anatomy.
Answer:
Ovary Of Introduction: Tire ovaries are a pair of female ^ reproductive glands, situated in the lesser pelvis. It is a female ♀ gonad which fonns the ova.
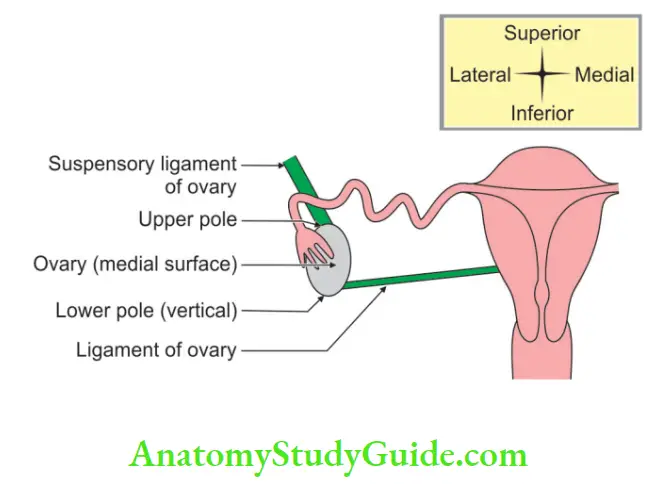
1. ovary Gross Anatomy:
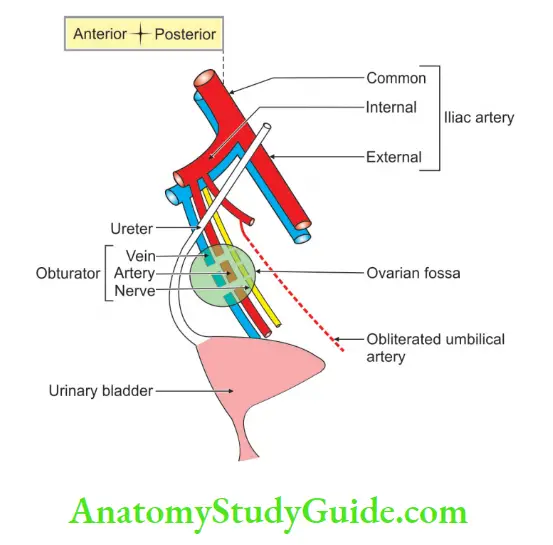
1. Situation: It is located in the ovarian fossa.
2. Dimension: 3 x 1.5 x 1 cm (length x breadth x thickness).
3. External features
- Surfaces:
- Medial, and
- Lateral.
- Borders:
- The Anterior or mesovarium border, and
- The posterior border is free border.
- Poles:
- Upper broader
- Lower narrower, and
- Axis:
- Multiparous: Horizontal.
- Nulliparous: Vertical.
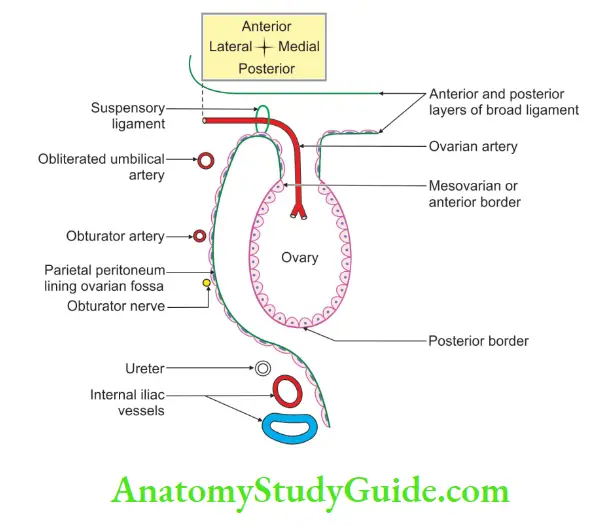
4. Prolapse Of Uterus Relations:
1. Peritoneal:
- Ovary is entirely covered with peritoneum except along the mesovarian border, i.e. anterior border where peritoneum is continuous with the posterior layer of broad ligament.
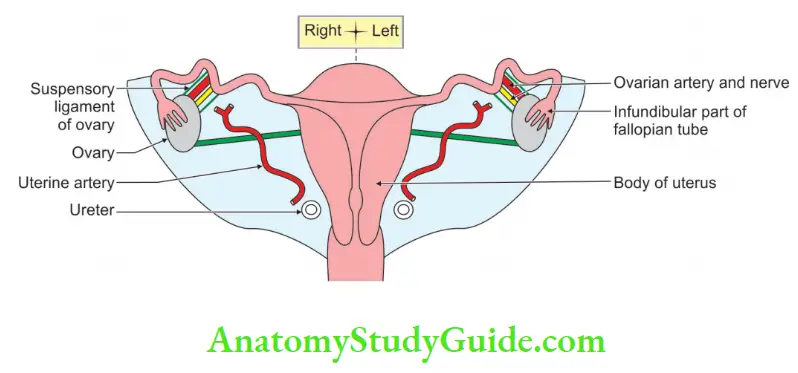
- Suspensory ligament of the ovary: It extends from upper pole of ovary to external iliac vessels. It contains ovarian vessels.
2. Visceral:
- Upper pole is related to uterine tube and external iliac veins.
- Lower pole is related to pelvic floor.
- Anterior border is related to uterine tube and obliterated umbilical artery.
- Posterior border:
- Uterine tube
- Ureter.
- Lateral surface: Ovarian fossa is related to obturator vessels and obturator nerve is separated by peritoneum, which is lined by parietal peritoneum.
- Medial surface: Uterine tubes.
5. Prolapse Of Uterus Blood supply:
1. Anterior supply:
- The ovary is supplied by the ovarian artery.
- It is a branch of the abdominal aorta arising just below the renal artery.
- The artery runs down behind the peritoneum.
- It crosses the ureter obliquely and crosses the brim of the pelvis.
- It enters the suspensory ligament.
- It gives a branch to the uterine
The tube which runs between the two layers of the broad ligament. It anastomoses with the uterine artery.
2. Venous drainage:
- The ovarian veins form a plexus in the mesovarian and the suspensory ligament which is called pampiniform plexus.
- The plexus drains into a pair of ovarian veins that accompany the ovarian artery.
- They usually combine as a single trunk before their termination.
- The right ovarian vein opens into the inferior vena cava. The left ovarian vein opens into the left renal vein.
6. Nerve supply:
It is formed by the ovarian plexus. The fibers of the plexus are formed
- Sympathetic fibers: Sympathetic fibers reach the ovary from the aortic plexus. The fibers run along its blood vessels. The pre-ganglionic fibers arise from the T10 and T11 segments of the spinal cord.
- Parasympathetic fibers: Parasympathetic fibers may reach the ovary from the inferior hypogastric plexus via the uterine artery.
- Sensory fibers: Sensory fibers accompany the sympathetic nerves so that the ovarian pain may be referred along the umbilicus.
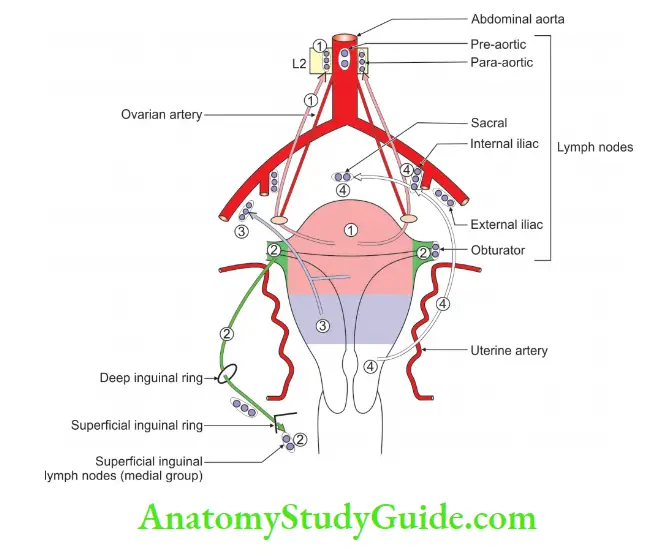
7. Lymphatics Drainage:
The lymphatics of the ovary drain to para-aortic nodes alongside the origin of the ovarian artery.
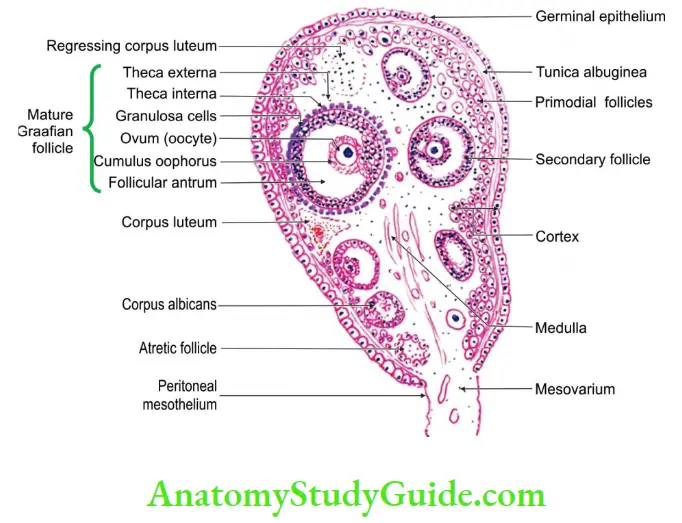
2. Histology
It shows the following layers from inside out
- Simple cuboidal epithelium
- Tunica albuginea, is a thin layer of connective tissue.
- The cortex contains ovarian follicles at various stages of development.
- Each follicle contains one oocyte.
- One follicle matures every month and sheds an oocyte.
- There are 400 oocytes that are ovulated in the reproductive life.
- After the oocyte is liberated, the Graafian follicle is converted into a structure called the corpus luteum.
3. Development
Chronological age: It develops in the 7th week of intrauterine life.
Germ layer: Endoderm.
Site: Wall of the yolk sac close to the allantois.
Sources:
1. Ovary develops from the coelomic epithelium lining the medial side of the nephrogenic cord.
2. The surface epithelium of the female ♀ gonad forms cortical cords.
3. In the 4th month of intrauterine life, these cords form primitive germ cell.
4. Descend of the gonads is considerably less in the female ♀ than male ♂.
5. The ovary is settled just below the rim of the true pelvis.
4. Applied Anatomy:
- Prolapse of ovaries: It is frequently displaced in the pouch of Douglas. It can be palpated by vaginal examination. The carcinoma of the ovary is common and accounts for 15% of all cancers and 20% of gynecological cancers.
- Krukenberg’s tumor: It is trans coelomic migration of cancer cells from the mammary gland to the ovary and forms a tumor called Krukenberg’s tumor.
- Oophoritis: It is the inflammation of the ovary. It may produce localized peritonitis of the ovarian fossa and eventual irritation of the obturator nerve. This results in pain on the medial side of the thigh.
Ovarian Fossa
Ovarian Fossa Introduction:
It is a fossa present in the pelvis which contains the ovary, the female gonad.
- Ovarian Fossa Boundaries:
It is bounded
1. Anteriorly by the obliterated umbilical artery.
2. Posteriorly
- Ureter, and
- Internal iliac artery
2. Ovarian Fossa Applied Anatomy:
The relationship of the obturator nerve to the ovarian fossa needs to be remembered.
1. The lateral surface of the ovary is in contact with the parietal peritoneum of the ovarian fossa.
2. The obturator nerve and vessels are retroperitoneal structures in this location.
3. Inflammation of the ovary may produce localized peritonitis in the ovarian fossa.
4. It causes irritation of the obturator nerve.
5. The patient may experience pain along the medial side of the thigh and knee.
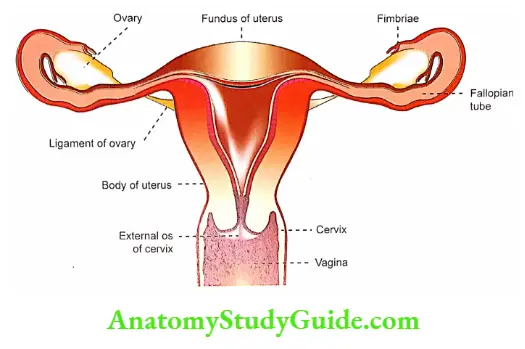
Question – 2: Describe the uterine tube under the following heads
1. Gross anatomy
2. Histology
3. Development, and
4. Applied anatomy.
Answer:
Uterine Tube Introduction:
These are the tortuous ducts that convey the ova from the ovary to the uterus.
The spermatozoa introduced into the vagina pass into the uterus and then into the uterine tubes.
The fertilization usually takes place in the ampullary part of the fallopian tube.
Length: About 10 cm (4″).
1. Uterine Tube Gross Anatomy:
1. External features: Parts of the uterine tube are as follows.
- Infundibulum: It is a funnel
 shaped lateral end of the uterine tube.
shaped lateral end of the uterine tube.
- It bears finger-like processes called fimbriae.
- It is, therefore, called a fimbriated end.
- One of the fimbriae is longer than the others and is attached to be tubal pole of the ovary.
- It is known as ovarian fimbriae.
- At the lateral end, the uterine tube opens into the peritoneal cavity through its abdominal ostium.
- It is about 3 mm in diameter.
- Ampulla: It is a thin-walled, dilated, and tortuous part of the fallopian tube. It forms approximately lateral two-thirds of the tube. It is about 4 mm in diameter.
- Isthmus: It is narrow, rounded, and cord-like.
- The interstitial part of the tube is about 1 cm long and lies within the wall.
2. Uterine Tube Course and Relations:
1. The ampulla arches over the ovary and is related to the anterior and posterior borders of the ovary. It is also related to the upper pole and medial surface of the ovary.
2. The uterine tube lies in the upper free margin of the broad ligament of the uterus. The part of the broad ligament between the attachment of the mesovarian and the uterine tube is known as mesosalpinx.
3. Uterine Tube Blood supply:
- Arterial supply:
- Tubal branch of the ovarian artery. The tubal artery runs below the tube between the layers of the broad ligament.
- It anastomoses with the tubal branches of the uterine artery in the broad ligament.
- Tubal branch of uterine artery.
- Venous drainage: The veins run parallel with the arteries. The veins of the tube join the pampiniform plexus and drain into the uterine veins
4. Uterine Tube Nerve supply:
The uterine tubes are supplied by both the sympathetic and parasympathetic nerves.
- The sympathetic fibers are derived from the hypogastric plexuses. They are vasomotor in function.
- Parasympathetic fibers are derived from S2, S3, and S4. They inhibit peristalsis and produce vasodilatation.
5. Uterine Tube Lymphatic drainage:
- The lymphatics of the fallopian tube join the lymphatics of the ovary and drain into lateral aortic and para-aortic nodes.
- The lymphatics from the isthmus accompany the round ligament of the uterus and drain into the superficial inguinal nodes.
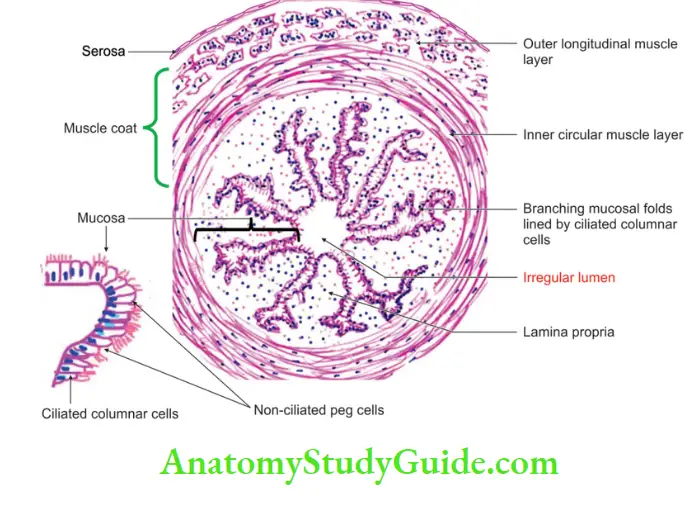
2. Uterine Tube Histology
It consists of
- Muscular coat: It consists of inner circular and outer longitudinal layers of the smooth muscle.
- The mucous membrane shows numerous branching fold which fill the lumen of the tube.
- Mucosa: It is lined by ciliated columnar epithelium.
3. Uterine Tube Development
Chronological age: It develops in the 8th week of intrauterine life.
Germ layer: Mesoderm.
Site: Intermediate mesoderm.
Sources:
- The proximal unfused vertical part of the paramesonephric duct forms the fallopian tube.
- Fimbriae are formed from the invagination of the paramesonephric duct into the coelomic epithelium.
Anomalies:
- Absence of the uterine tubes on one or both sides.
- The tubes may be partially or completely duplicated on one or both sides.
- There may be atresia in the tubes.
- Hydatid (of Morgagni): The cranial end of the paramesonephric duct does not contribute to the infundibulum of the uterine tube.
- It may persist as a vesicular appendage called hydatid of Morgagni.
4. Uterine Tube Applied Anatomy
- Salpingitis: Inflammation of the uterine tube is called salpingitis.
- Tubectomy: It removes a segment of the uterine tube on both sides. This is done in family planning operations. It can be done by laparoscopy or through an incision in the abdominal wall.
- Sterility: The inability to conceive or induce conception is called sterility.
- The most common cause of sterility in the female ♀ is blockage of the fallopian tube.
- It may be congenital or may be acquired by tuberculosis infection. The patency of the tube is investigated by
- Chromopertubation: It is a method for the study of the patency of the fallopian tube in suspected infertility in women.
- It is currently one of the standard procedures in the field.
- Hysterosalpingography: It is a radiological technique.
-
- A radio-opaque oily dye is injected into the uterus through the cannula.
- It helps to visualize the cavity of the uterus and the lumina of the tubes. It helps to find out the patency of tubes.
Question 3: What is hysterosalpingography?
Answer:
Hysterosalpingography: It is a radiological technique. A radio-opaque oily dye is injected into the through the cannula. It helps to visualize the cavity of the uterus and the lumen of the tubes. It helps to find out the patency of tubes.
Applied Importance Of Supports Of Uterus.
Supports of the uterus keep the uterus in position. Weakness of the supports results in prolapse of the uterus.
Abnormal Positions Of Uterus
1. Dextrorotation of the fundus: The uterus lies in the median plane. It is twisted in the long axis either to the right or left.
2. Levo (left) rotation: The Cervix is tilted more to the left side and comes closer to the left ureter.
Dextrorotation and levorotation take place in the anteroposterior axis which passes through internal os.
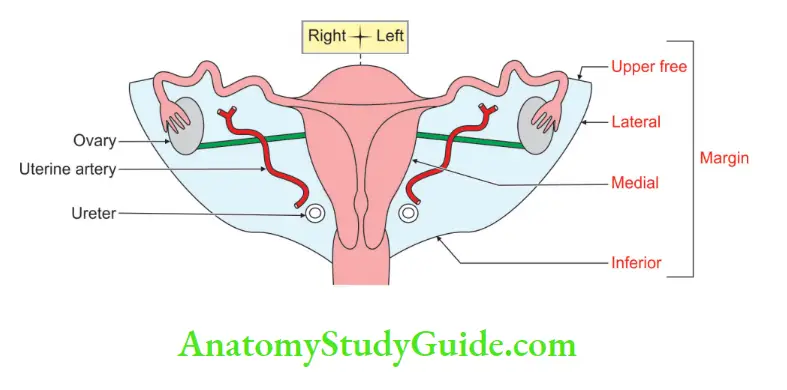
Broad Ligament Of Uterus
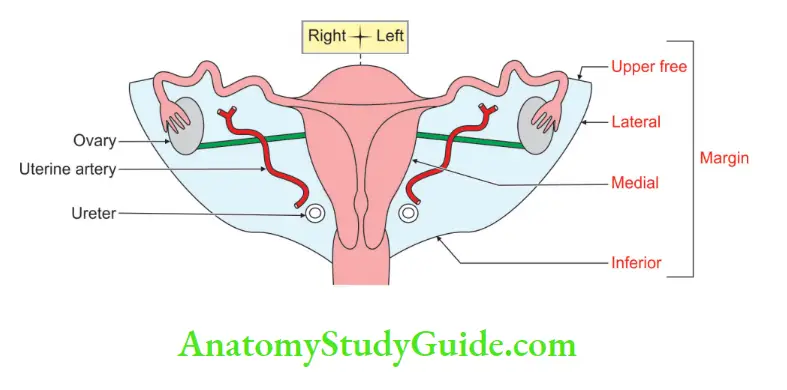
1. It is a fold of the peritoneum extending from the body of the uterus to the lateral pelvic wall. It has
- Two layers: Anterior and posterior layers.
- Margins:
- Lateral and
- Superior free margins.
2. Structures in broad ligament and their position in the broad ligament.
- Fibrofatty tissue between two layers is called parametrium.
It is most abundant near the cervix and vagina:
- Fallopian tube in the upper free margin.
- A round ligament of the uterus is present in the anterior inferior part of the broad ligament.
- The ligament of the ovary is present in the posterior inferior part of the broad ligament.
- The uterine artery ascends between two layers of the broad ligament.
- Ovarian vessels
- Utero-vaginal and ovarian nerve plexus.
- Lymph nodes and lymph vessels
- Remnants of Wolffian duct or mesonephric duct Epoophoron Paroophoron, and Gartner’s duct
Not but yes content of broad ligament:
Note: Anatomically, the ureters are not content of broad ligament. In growing tumors, they may be pushed and can be contents of broad ligaments.
3. Parts of broad ligament:
- Mesosalpinx: Part of the broad ligament between the uterine tube and mesovarian.
- Mesovarian: The ovary is attached to the posterior layer of the broad ligament.
Question 4: Describe the uterus under the following heads
1. Gross anatomy
2. Histology
3. Development, and
4. Applied anatomy.
Uterus Of Introduction: It is a child-bearing organ present in the pelvic cavity.
1. Gross Anatomy
1. External features
1. Axis of uterus:
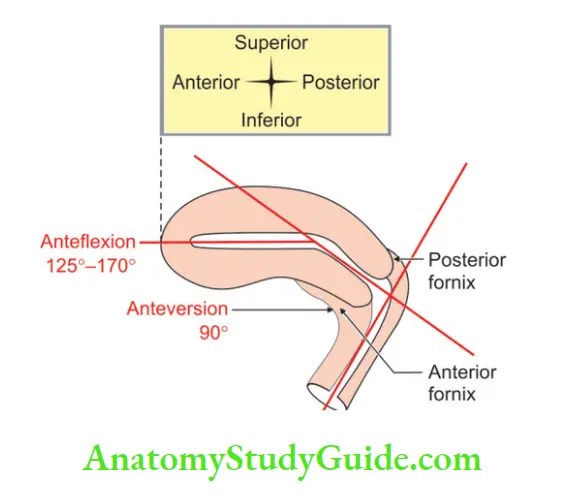
- Anteversion: (ante—prior to or in front of, version—relation of the uterus with the vagina around a transverse axis through external os of the cervix)
- It is the forward lipping or tilting of an organ.
- It is the displacement of the organ.
- It is tipped forward but not bent at an angle as occurs in anteflexion.
- However, it is defined as the forward angle between the axis of the cervix and that of the vagina, measuring 90°.
- Anteflexion: Forward angle between the body and the cervix, at the isthmus. It measures 135°, provided the bladder and rectum are empty.
2. Supports of the uterus: The most fixed part of the uterus is the cervix. The urinary bladder and vagina maintain the position of the uterus, example distention of the bladder makes the uterus erect and lies in the same line as a vagina. This position favors the prolapse of the uterus. The following are the main supports.
Axis: The maintenance of the anteversion axis is an important pre-requisite for the support of the uterus.
Perineal body:
- It is a pyramidal
 shaped fibromuscular node and is formed by paired and unpaired muscles.
shaped fibromuscular node and is formed by paired and unpaired muscles. - Functions: It maintains the integrity of the pelvic floor.
Muscles:
Levator ani which is formed by
- Pubovaginalis, and
- Puborectal sling.
Functions of levator ani
- It constricts the vagina from the side and maintains the anorectal flexure.
- It prevents the prolapse of the uterus.
- In a damaged puborectal sling, the anorectal angulation becomes straight and this results in prolapse of the rectum.
Ligaments: These are minor supports.
- Mackendrodt’s ligament: It keeps the cervix in the midline. It prevents the downward displacement of the uterus through the vagina.
- Uterosacral ligament: It is a condensation of pelvic fascia that extends from the cervix.
- It embraces the rectouterine pouch and attaches to the fascia over the piriformis.
- It is best palpated in rectal examination.
- It keeps the cervix braced backward against the forward pool of the round ligaments on the fundus.
- And so, maintain the body of the uterus in ante-version.
3. Pubocervical ligament: It prevents excessive traction of the cervix by counteracting the uterosacral ligament. It keeps the cervix in position. Broad ligaments of the uterus
The tone of the muscles of the abdominal wall maintains intra-abdominal pressure. In the weakness of the muscle tone, the sigmoid colon and small intestine exert pressure upon the uterus.
Know what is not—Important:
Note: Peritoneal folds do not play a role in maintaining the support of the uterus.
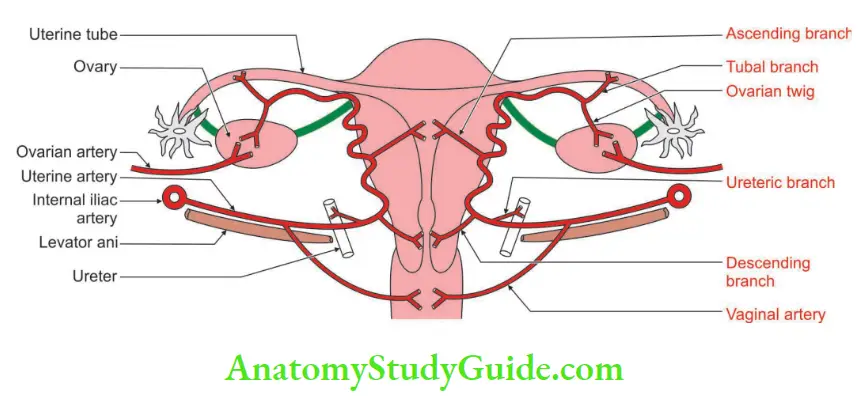
2. Blood supply:
- Arterial supply: It is chiefly by uterine arteries, which are branches of the anterior division of the internal iliac artery. They are tortuous in course for the expansion of the uterus during pregnancy. They give > arcuate artery > radial artery > spiral artery> basilar artery.
- Venous drainage: The veins of the uterus form a plexus along the lateral border of the uterus. The plexus drains through the uterine, ovarian, and vaginal veins into the internal iliac veins> common iliac > inferior vena cava.
3. Nerve supply: The uterus is richly supplied by both sympathetic and para-sympathetic nerves, through the inferior hypogastric and ovarian plexuses.
- Sympathetic nerves (T12, L1) produce uterine contraction and vasoconstriction.
- Parasympathetic nerves (S2, S3, S4) produce uterine inhibition and vasodilatation.
However, these effects are complicated by the pronounced effects of hormones on the genital tract. Pain sensations from the
- The body of the uterus passes along the sympathetic nerves.
- The cervix passes along the parasympathetic nerves.
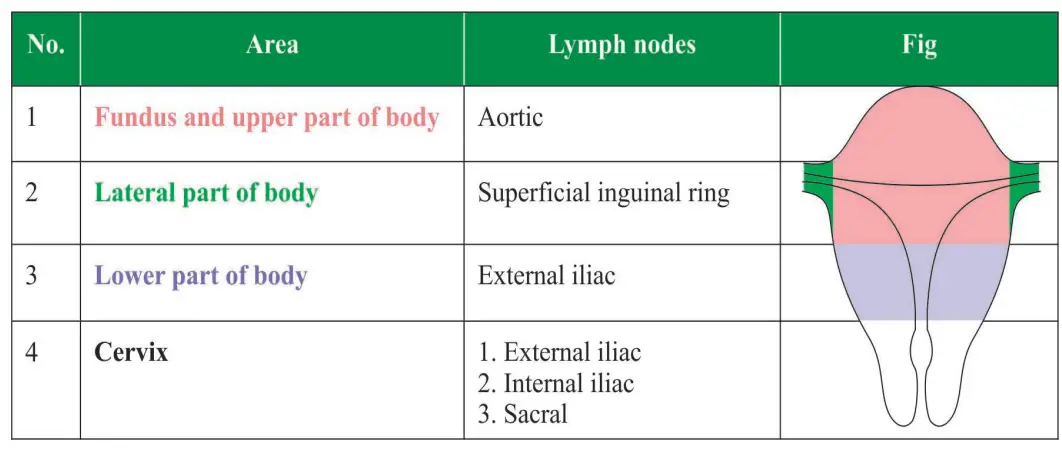
4. Lymphatic drainage:
1. The lymphatics pass with each vein to the internal iliac group of lymph nodes.
2. The lymphatics of the uterus form three inter-communicating networks: Endometrial, myometrial, and subperitoneal.
3. These plexuses drain into lymphatics on the side of the uterus. The lymphatics of the uterus are displayed
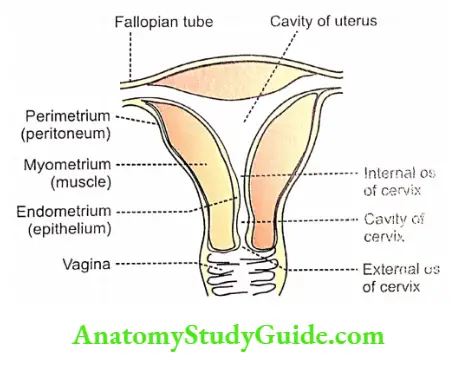
2. Uterus Histology
Endometrium:
- The mucous membrane of the uterus is called the endometrium.
- It is lined by the simple columnar epithelium.
- It rests on the connective tissue.
Lymphatic drainage of the uterus:
- It shows numerous tubular glands which are dipped into the stroma.
- The appearance of the endometrium varies depending on the phase of the menstrual cycle.
- In the proliferative phase, the endometrium is relatively thin and the glands are straight.
- In the secretory phase, the endometrium is much thicker.
- The uterine glands are long dilated and tortuous.
- They show a saw-toothed margin in the section.
- The blood vessels are more conspicuous.
The stroma is divisible into three parts:
- The superficial layer is called the stratum compactum in which the cells are closely packed.
- Middle stratum spongiosum, which is relatively loose.
- Stratum basale in which the cells are densely packed.
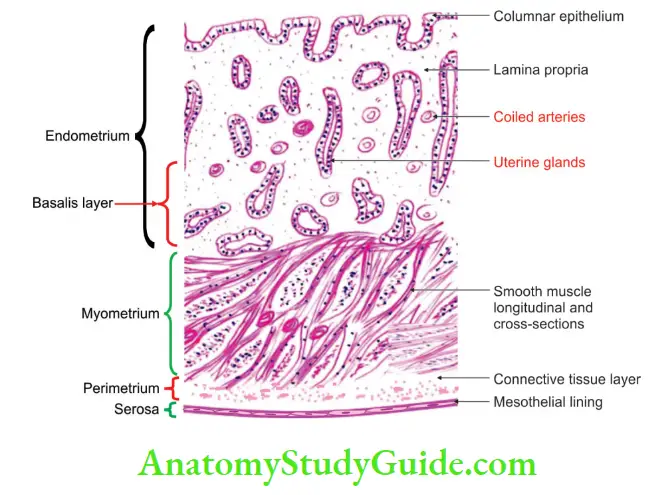
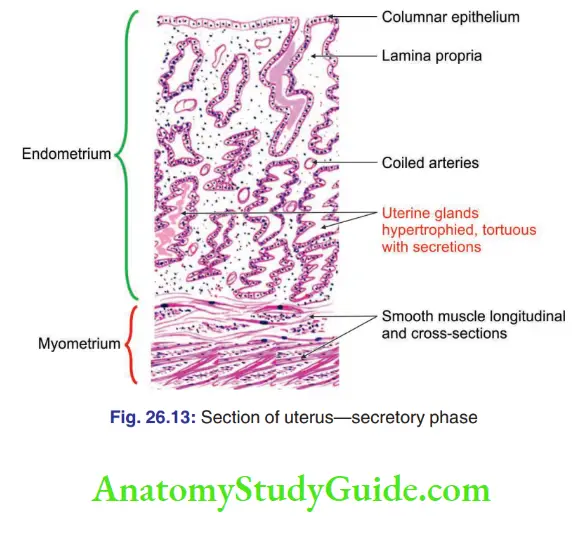
Myometrium:
- The middle thick layer is formed by smooth muscles. It is called myometrium.
- It consists of various layers. But these are difficult to make out as fibers run in various directions.
- Perimetrium: The outer layer is the perimetrium.
3. Uterus Development
Chronological age: It develops in the 8th week of intrauterine life.
Germ layer: Mesoderm.
Site: Intermediate mesoderm.
Sources:
- Epithelium of the uterus develops from the fused paramesonephric ducts.
- The myometrium is derived from the surrounding mesoderm.
- The caudal unfused part partially gets embedded within the substance and forms the fundus of the uterus.
Anomalies:
1. Common anomaly:
- Uterus bicornuate: It is one of the relatively common anomalies of the uterus.
- The uterus has two horns entering a common vagina.
2. The less common anomalies are
The lumen may be partially or completely subdivided by a septum.
- The entire uterus may be absent.
- One-half of the uterus may be absent (unicornuate uterus).
- The uterus may remain rudimentary.
- There may be atresia of the lumen either in the body or in the cervix.
- The cervix may be absent.
4. Uterus Applied Anatomy:
- Sometimes the uterus passes downwards into the vagina which is called prolapse of the uterus.
- It is caused by the weakness of the various supports of the uterus.
- Hysterectomy is the operation for the removal of the uterus.
- Insertion of a foreign body into the uterus can prevent implantation of a fertilized ovum.
- This is the basic principle underlying the use of various intrauterine contraceptive devices.
- Caesarean section: The delivery of the child is done by opening the abdomen and uterus.
- It is commonly done for the cephalopelvic disproportion.
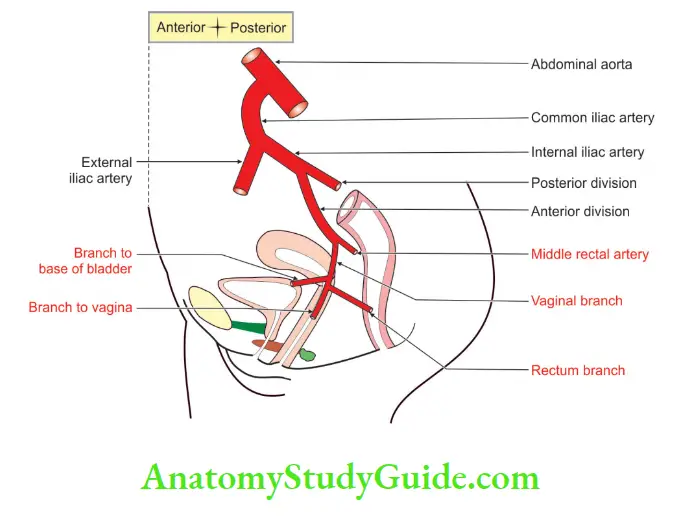
Uterine Artery
Introduction: The uterine artery is present only in females ♀ It is the chief artery of the uterus. It is homologous to the artery to the ductus deferens in males ♂
1. Uterine Artery Origin: It is a large artery that springs from the anterior division of the internal iliac artery below the obturator artery.
2. Uterine Artery Course And Relations:
- It has a C-shaped course in the pelvis.
- It is directed downwards and medially on the levator ani muscles and crosses the ureter.
- The points at this site are as follows
- This is the most dangerous site.
- The ureter is likely to be damaged during a hysterectomy because of the following reasons
- The uterine artery crosses from lateral to medial.
- The uterine artery crosses the ureter from the front.
- It is described as “water under the bridge” by surgeons.
- In this simile, water is the ureter and the bridge represents the uterine tube.
- However, the author feels it is better to call it a ‘Urine tube under a blood tube’.
- It is 1” lateral to the cervix.
- It is above the Mackendrodt’s ligament.
-
- It runs along the lateral border of the body.
- It runs in a very tortuous manner, lying between the two layers of the broad ligament.
3. Uterine Artery Branches:
Close to the area of crossing, the artery gives
1. Ureteric
2. Vaginal, and
3. Cervical branches.
The cervical branches form circular anastomosis around the isthmus.
4. On reaching the side of the cervix, the uterine artery divides into two branches.
- A smaller descending vaginal branch supplies the cervix and vagina.
- A larger ascending branch runs along the lateral margin of the uterus.
5. Along the fallopian tube, it gives off tubal branches and a few ovarian twigs.
6. The ascending branch gives a series of arcuate or coronary arteries. They run transversely on the anterior and posterior surfaces of the body of the uterus.
7. The branches of the two sides are anastomose with their counterparts in the midline.
8. Numerous radial arteries arise from the coronary arteries.
9. They pierce the myometrium centripetally and anastomose with each other to form stratum vasculare in the middle layer of the muscular coat.
10. From stratum vasculare, two sets of branches—basal and spiral—arise to supply the endometrium.
11. The functional zone of the endometrium is cast off during menstruation and is supplied by the spiral arteries.
12. Whereas the basal zone of the endometrium helps in the regeneration of the denuded endometrium and is supplied by basal arteries.
Dil Mange more:
Please note important additional information about the uterine artery.
- The uterine artery is one of the tortuous arteries in the body.
- It hypertrophies, i.e. greatly enlarged during pregnancy.
- Muscular branches of the uterine muscle are also tortuous and are known as helicine arteries.
- The muscle bundles in the myometrium layer are arranged in a figure-8 design and hence on their contraction blood vessels are clamped.
- This is the reason why these muscle fibers are known as living ligatures of the uterus.
4. Uterine Artery Distribution:
The uterine artery supplies
1. Ureter
2. Vagina
3. Uterus
4. Medial two-thirds of uterine tube
5. Ovary, and
6. Structures within the broad ligament, i.e.
- Round ligament of the uterus, and
- Ligament of the ovary.
Additional responsibility: Please note that it also supplies the placenta during pregnancy.
5. Uterine Artery Anastomosis:
- The uterine artery forms anastomosis with
- The vaginal artery, it forms two trunks in front and behind the vagina.
- They are known as azygos arteries of the vagina.
- Cervical branches form circular anastomosis around the isthmus.
- Fellow of the opposite side of the body of the uterus.
- The ovarian artery at the medial end of the uterine tube.
6. Uterine Artery Applied Anatomy:
1. The branches of the uterine artery diminish rapidly in size as they pass toward the uterine cavity.
2. Hence, there is relatively little bleeding in the midline section of the uterus.
3. It is essential to know that the ureter is identified at the base of the broad ligament.
4. The uterine artery crosses the ureter approximately 2 cm superior to the ischial spine.
5. The ureter is in danger of being inadvertently clamped during a hysterectomy. Hence, care should be taken not to injure the ureter during ligation of the uterine artery.
6. In cases of dextrorotation of the fundus, the cervix is tilted more to the left side and becomes closer to the left ureter.
7. Hence, one should be more cautious while ligating the left uterine artery.
Middle Rectal Artery
1. Middle Rectal Artery:
The middle rectal artery is characterized by the following features
- It is known for its variation in presence, origin, size, and distribution.
- It is often absent, multiple, or maybe small.
- In males ♂ , it may be replaced by a branch from the inferior vesical artery.
- In females ♀ it may be replaced by a branch from the uterine or vaginal artery.
2. Middle Rectal Artery Origin: It arises from the internal iliac artery. The origin is close to the inferior vesical artery.
3. Middle Rectal Artery Course:
- It runs into the lateral fascial coverings of the mesorectum.
- It anastomoses freely with the arteries of the opposite sides.
- It has a poor anastomosis with the
- Superior rectal artery, which is a continuation of the inferior mesenteric artery, and
- Inferior rectal artery is a branch of the internal pudendal artery.
4. Middle Rectal Artery Distribution:
1. In males ♂ , it mainly supplies the
- Seminal vesicles
- Vas deferens, and the
- Prostate
2. In females ♀ it supplies the vagina
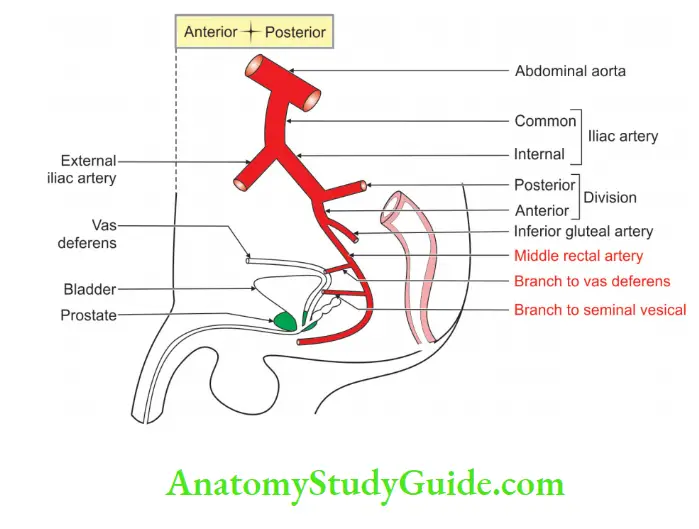
3. In males ♂ and females ♀ it supplies
- Only the muscle coat of the middle 1/3rd of the outer coats of the rectum
- The mucous membrane of the anal canal, and
- Muscle of the upper part of the anal canal.
Female Reproductive Organs
The female reproductive system comprises primary sex organs and accessory sex organs.
Primary Sex Organs
The primary sex organs are a pair of ovaries, which produce eggs or ova and secrete female sex hormones, estrogen, and progesterone. Details of structure and functions of ovary.
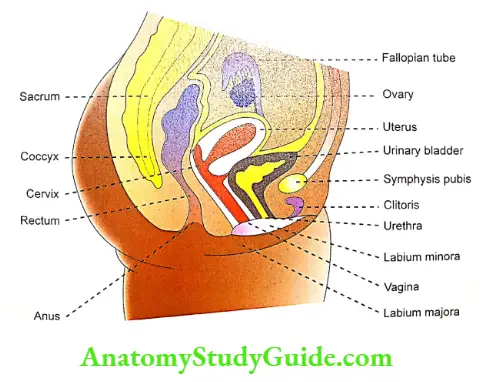
Accessory Sex Organs
The accessory sex organs in females are:
- A system of genital ducts: Fallopian tubes, uterus, cervix, and vagina
- External genitalia: Labia majora, labia minora and clitoris.
The mammary glands are not the female genital organs but are the important glands of the female reproductive system.
Functional Anatomy Of Accessory Sex Organs
Uterus
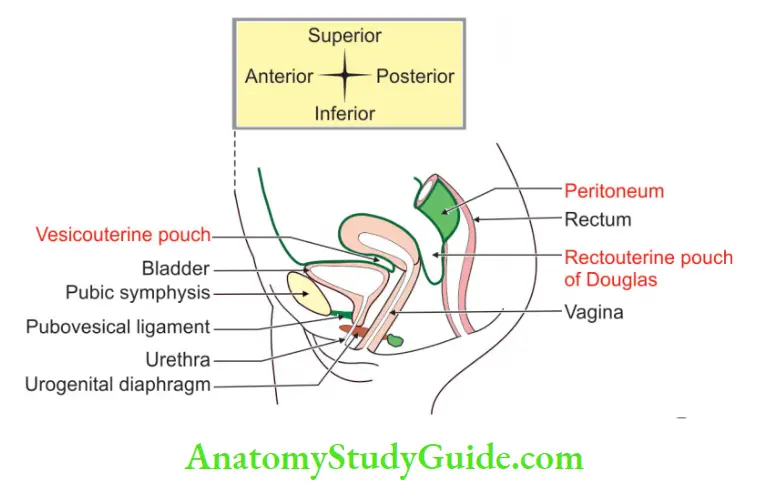
- The uterus is otherwise known as the womb. It lies in the pelvic cavity between the rectum and urinary bladder. The uterus is a hollow muscular organ with a thick wall.
- It has a central cavity that opens into the vagina through the cervix. On either side at its upper part, the fallopian tubes open. The uterus communicates with the peritoneal cavity through fallopian tubes.
- The virgin uterus is pyriform in shape and is flattened anteroposteriorly. It measures about 7.5 cm in length, 5 cm in breadth at its upper part, and about 2.5 cm in thickness.
There is a constriction almost at the middle of the uterus called an isthmus. It divides the uterus into two portions:
- The portion above the isthmus called the body of the uterus
- The portion below the isthmus is called the cervix.
The dome-shaped part of the body which lies above a plane passing through the points of entrance of the fallopian tubes is known as the fundus.
Structure of uterus
The uterus is made up of 3 layers:
- Outer serous layer
- The middle muscular layer or myometrium
- Inner mucus layer or endometrium.
1. Outer Serous Layer
It is the covering of the uterus derived from the peritoneum. Anteriorly, it covers the uterus completely but posteriorly it covers only up to the isthmus.
2. Middle Muscular Layer Or Myometrium
This layer is the thickest of all layers. It is made up of smooth muscle fibers which are divided into three different groups.
- External myometrium in which the muscle fibers are arranged transversely
- Middle myometrium in which the muscle fibers are arranged longitudinally, obliquely, and transversely
- Internal myometrium which is formed by circular muscle fibers.
The muscular layer is interposed with blood vessels, nerve fibers, lymphatic vessels, and areolar tissues.
3. Inner mucus layer or endometrium
- It is smooth and soft with pale red color. It is made up of ciliated columnar epithelial cells. Minute orifices are found on the surface of the endometrium. The tubular follicles of endometrium open through these orifices.
- The endometrium also contains connective tissue in which the uterine glands are present. Uterine glands are lined by ciliated columnar epithelial cells.
Changes in uterus
- The uterus changes its size, structure, and function lr, different phases of sexual life. Just before menstruation, the uterus is enlarged and becomes more vascular.
- The endometrium thickens with more blood supply. This layer is desquamated during menstruation and reformed after menstrual period.
- During pregnancy, the uterus is enlarged very much with an increase in weight. After parturition (delivery), it comes back to its original size but the cavity remains larger. In old age, the uterus is atrophied.
Cervix
The cervix is the lower constricted part of the uterus. It is divided into two portions:
- Upper supravaginal portion
- Lower vaginal portion
The supravaginal portion communicates with the body of the uterus through the internal os (orifice) of the cervix. The vaginal portion of the cervix projects into the anterior wall of the vagina and it communicates with the vagina through the external os (orifice) of the cervix.
The mucous membrane of a supravaginal portion of the cervix has many glandular follicles, which secrete mucus. The mucus membrane of the vaginal portion is formed by stratified epithelial cells.
Vagina
The vagina is a short tubular organ. It is lined by mucous membrane which is formed by stratified epithelial cells.
Sexual Life In Females
The lifespan of a female is divided into three periods.
First Period
It extends from birth to puberty. During this period, primary and accessory sex organs do not function. These organs remain quiescent. Puberty occurs at the age of 12-15 years.
Second Period
The second period extends from the onset of puberty to the onset of menopause. The first menstrual cycle is known as menarche. The permanent stoppage of the menstrual cycle in old age is called menopause, which occurs at the age of about 45-50 years. During the period between menarche and menopause, women menstruate and reproduce.
Third Period
This period extends after menopause to the rest of your life.
Leave a Reply