General And Local Examination Introduction
A holistic examination of the patient leads to a specific diagnosis and corresponding treatment planning. An overview of the patients obtained by general examination. The examination of a patient includes the following steps:
Table of Contents
- Inspection: Careful visualisation
- Palpation: Touch and feel
- Percussion: Tap and feel
- Auscultation: Amplify to hear
Read And Learn More: Paediatric Dentistry Notes
In dentistry, the local examination is the examination of the head and neck region, especially the orofacial apparatus. It is further split into intraoral and extraoral examinations.
The intraoral examination includes the examination of the hard and soft tissues. A paediatric patient can be examined only when he/she cooperates. The questions pertaining to the case history cannot always be asked to the patient as he/she may not have the cognitive ability to reply.
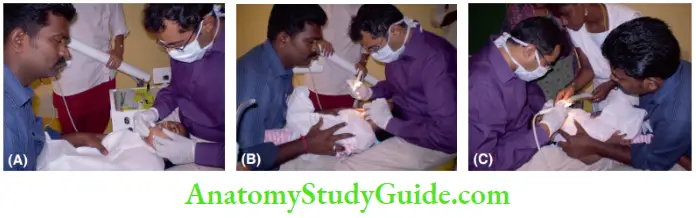
- (A) The child is able to interact with the parent and the dentist.
- (B) The dentist can directly visualise the oral cavity of the child who is at a slightly higher level than the parent. The immobilisation of the child’s extremities is done by the parent. The legs of the child are laid each on one side of the parent who restrains him with his elbow.
- (C) The parent holds the hands of the child to reassure and restrain him. The dental assistant is on the non-working side of the dentist.
The method of examining a paediatric patient depends on the age of the patient. A child younger than 2 years has to be examined in a lap-to-lap or knee-to-knee position.
The parent and the dentist sit on either side with the child on their lap. A 2–3-year-old child may be examined in a patient-over-parent mode. A patient older than 3 years can be examined in the dental chair. Questions may be asked to the patient older than 4 years. The language and the choice of words should be comfortably understood by the patient.
General examination
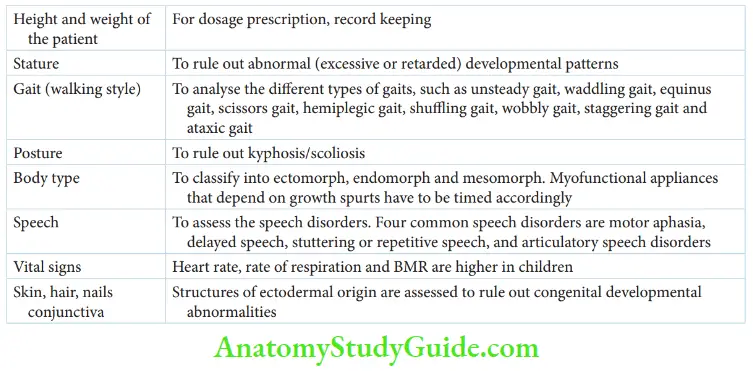
The general appraisal of the patient is called a general examination. It gives a primary conclusion of the overall health of the patient. The general examination includes an assessment of the height, weight, stature (posture), gait (walking style), body type and speech. It also includes the examination of skin, nails and conjunctiva.
- Height and weight: Th height and weight of the patient is recorded to complete the history. The dosage of any drug in the prescription depends on the weight of the patient. The height of the patient is required to compute the body surface area. Body surface area is the most appropriate parameter to compute drug dosage.
- Stature: Children who are too short or too tall for their age may be suspected for abnormal (excessive or retarded) developmental patterns. Factors such as heredity, nutritional intake, socioeconomic environment, developmental anomalies and metabolic disturbances can be probed to reveal the cause of the abnormality.
- Gait: Th gait or the style of walking of the child has to be observed for any abnormality. Some abnormal gaits and their corresponding conditions are given.
- Different Patterns of Abnormal Gait Unsteady gait – General weakness of a febrile child
- Waddling gait – Cerebellar dysfunction
- Equinus gait – Cerebellar dysfunction
- Scissors gait – Systemic fluorosis
- Hemiplegic gait – Cerebral palsy
- Shuffling gait – Cerebral palsy
- Wobbly gait – Cerebral palsy
- Staggering gait – Cerebral palsy
- Ataxic gait – Cerebral palsy
- Different Patterns of Abnormal Gait Unsteady gait – General weakness of a febrile child
- Posture: Normally, a person should maintain an erect posture. It may be altered in the case of kyphosis (forward bending of the spine) or scoliosis (lateral bending of the spine).
- Body type: Th child may be ectomorphic (tall and thin body type), endomorphic (short and stout body type) or mesomorphic (average body type). Endomorphs attain puberty earlier (early maturers) than ectomorphs (late maturers). Hence, the associated growth spurt at puberty is earlier than that in ectomorphs. When my functional appliances that target the pubertal growth spurt are indicated to such children, they have to be timed appropriately.
- Speech: Normally, a child starts conversing in sentences by 2 or 3 years of age. The speech has to be assessed for any abnormality. Some common speech disorders are listed.
- Common Speech Disorders
- Motor aphasia: Loss of speech secondary to central nervous system damage
- Delayed speech: Early hearing loss, intellectual retardation, general developmental retardation, sensory defects and lack of motivation
- Stuttering or repetitive speech: Cerebral palsy, neurodevelopmental disorders and compulsive disorders
- Articulatory speech disorders such as substitution, omission, insertion and distortion.
- Common Speech Disorders
- Vital signs: Th vital signs including the heart rate and respiratory rate are recorded. The values are higher than the normal adult values.
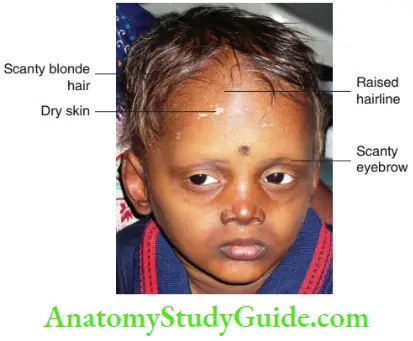
- Structures of ectodermal origin: Skin, nails, hair, conjunctiva and teeth are structures of ectodermal origin. Developmental disturbances in the skin, nails and conjunctiva can reveal associated disturbances of teeth as they arise from the same origin.
- Skin is assessed for abnormalities such as increased temperature, excessive moisture and dryness. The hair distribution is also observed. Inspection may reveal primary and secondary skin lesions such as macules, papules, vesicles, ulcerations, crusts and scales. If these lesions are found, exanthematous diseases, vitamin deficiencies and developmental disturbances have to be suspected. A physician has to be referred in case of any abnormality.
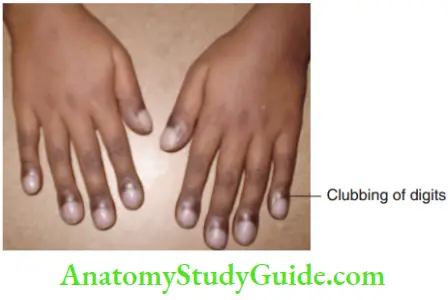
- The nails of the child have to be observed carefully. Some children may display abnormal oral habits such as nail biting or thumb sucking. The nails may be bitten or appear irregular when the child has a nail-biting habit. A thumb-sucking child will display diligently clean nails and digits with or without a callus. Nails may be spoon-shaped in an anaemic child while they may be pitted, brittle, scaly, thickened or even absent in ectodermal disturbances. Clubbing of the digits can be noticed in a child suffering from cyanotic congenital heart disease
- The hair of a child can reveal many abnormalities. The distribution of hair has to be observed. Hair may be scanty and lighter in colour in case of ectodermal dysplasia. Alopecia may be occasionally seen in younger patients. Loss of hair or baldness with an indurated and inflamed line is characteristic of ringworm infection. Hormonal imbalances may cause loss of hair. Certain medications such as phenytoin (anticonvulsant), cyclosporine (immunosuppressant), androgenic steroids and progesterone (used in hormone imbalances) can cause hirsutism or excessive hair growth.
- Conjunctiva can be examined for anaemia or jaundice. Paleness of conjunctiva is observed in anaemia and yellowness of conjunctiva indicates jaundice. However, biochemical investigations are confirmatory tests.
Local Examination
In dentistry, local examination pertains to the examination of the orofacial apparatus. It encompasses extraoral and intraoral examinations.
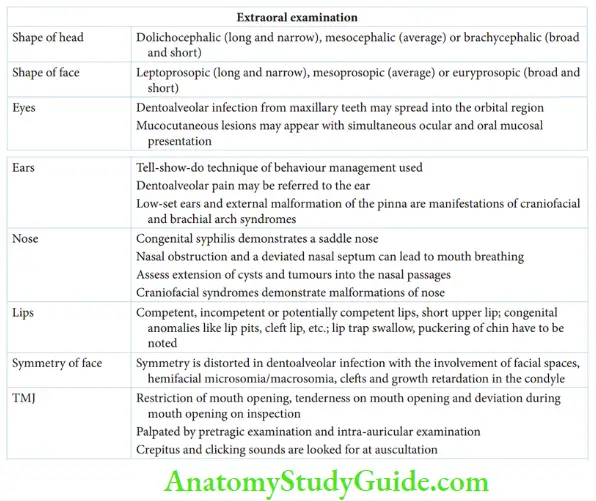
- Extraoral Examination The extraoral examination includes the examination of the following structures:
- The shape of the head: Shape is assessed by inspecting the head. The anteroposterior dimension, extending from the frontal bone to the occipital bone, is the length of the head. The lateral extent, extending from one temporal bone to the other, is the breadth of the head. The shape of the head can be one of the following when seen from above:
- Dolichocephalic: Long and narrow head outline
- Mesocephalic: Average length and breadth
- Brachycephalic: Broad and short head outline
- The shape of the face: This corresponds to the shape of the head and can indicate whether the patient is ectomorph, endomorph or mesomorph.
- Leptoprosopic: A long and narrow face corresponding to the dolichocephalic head pattern indicates ectomorphs.
- Mesoprosopic: Average facial dimension corresponding to the mesocephalic head pattern indicates mesomorphs.
- Euryprosopic: A broad and short face corresponding to the brachycephalic head pattern indicates endomorphs.
- Eyes: Visual impairment or refractive errors of the child have to be recorded. The closure of the eyelid has to be observed. Other abnormalities such as swelling or puffiness around the eyes, crusting or lesions around the eyes, conjunctivitis, excessive lacrimation and hypertelorism may reveal many disease conditions.

- Significance Of Ocular Examination
- A child with a sensory handicap or blindness is classified as a special child. Strategic behaviour management is required to treat such a child. Sys systematic desensitisation (tell-show-do) is modi fid into touch-feel-do. The child is first allowed to touch the instrument; later, a chance is given to feel how it works before starting the treatment. For example, a child’s fist touches the aerator and the water spray from the aerator is later felt by the child. The treatment is performed after this.
- Dentoalveolar infection of the maxillary teeth may spread into the orbital region. This may lead to puffiness around the eyelids and conjunctivitis.
- Mucocutaneous lesions such as Behçet’s syndrome display ocular and oral mucosal lesions simultaneously.
- Puffiss around the eyelids and periorbital tissues may also result due to chronic upper respiratory tract infection, chronic sinusitis and allergy.
- Significance Of Ocular Examination
- Ears: Hearing impairment has to be recorded. History of earache or external auditory meatus discharge has to be enquired about. The external ear and the mastoid process have to be palpated for any tenderness.
- Significance Of Aural Examination
- A child with sensory impairment or deafness is classified as a special child. The tell-show-do technique is the behaviour management strategy adopted in such cases.
- Any dentoalveolar pain may be referred to the ear causing earache.
- A patient with an earache, not associated with dental fiding, has to be referred to an ENT specialist.
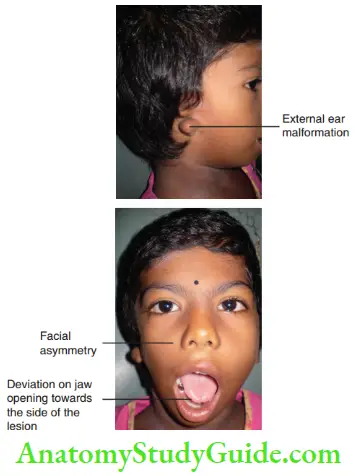
- Low-set ears and external malformation of the pinna are manifestations of various craniofacial and brachial arch syndromes such as Treacher– Collins syndrome and brachial-to-renal syndrome. In Treacher–Collins syndrome, bilateral symmetric external ear canal abnormalities are seen. Brachial-to-renal syndrome is a condition affecting the second brachial arch and causing ear and renal malformations.
 1. (A) Anomalous left ear with tags.
1. (A) Anomalous left ear with tags.
2. (B) Facial asymmetry.
3. (C) Anomalous formation of the pinna of the right ear.
- Significance Of Aural Examination
- Nose: Th type of breathing of the patient has to be observed. It can be nasal, oral or combined breathing. The water-holding test helps in confirming the observation. Any obstruction in the nasal passage has to be identified. History of serous, purulent or blood discharge from the nose has to be enquired about. Other anatomical defects such as depressed nasal bridge, asymmetry of nose, deviated nasal septum or scars due to trauma or surgery have to be recorded.
- Significance Of Nasal Examination
- The mouth-breathing habit of the child may be the result of nasal obstruction or a deviated nasal septum.
- Nasal discharge necessitates an ENT referral.
- Cysts and tumours originating from the maxilla may extend into the nasal passages.
- A saddle nose is observed in a child suffering from congenital syphilis.
- Craniofacial syndrome demonstrates various malformations of the nose.
- Significance Of Nasal Examination
- Lips: On extraoral examination, the lips are classified as competent, incompetent or potentially competent.
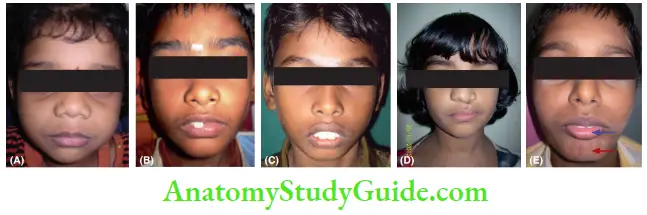 1. (A) Competent lips.
1. (A) Competent lips.
2. (B) Potentially competent lips due to malposition of the right central incisor.
3. (C) Short upper lip causing incompetent lips.
4. (D) Surgically corrected upper cleft lip.
5. (E) Lip trap swallow (blue arrow) with puckering of chin (red arrow).- Competent: Th lower lip is able to touch the upper lip effortlessly.
- Incompetent: Th lower lip has to be strained to contact the upper lip.
- Potentially competent: Dentoalveolar protrusion prevents the lip from being competent. It implies that the lips may become competent when the protrusion is corrected.
- Significance Of Lip Examination
- Congenital anomalies such as persisting cleft lip, congenital lip pits and double lip require correction.
- A short upper lip or hypotonic upper lip is associated with moderate-to-severe dentoalveolar protrusion. Lip exercises are indicated during therapy.
- Lip trap swallow is a condition where the lower lip is posturally trapped between the upper and lower incisors. It is associated with excessive overjet.
- The lips may exert protrusive force during swallowing. This causes contraction of the mentalis muscle displaying a ‘golf ball’ appearance during swallowing. This is also called puckering of the chin.
- Significance Of Lip Examination
- The symmetry of the face: Th apparent facial symmetry has to be assessed. Craniofacial abnormalities such as hemifacial microsomia or macrosomia or hypertrophy can cause asymmetry of the face. Cleft of the lip and palate and oblique facial cleft also affect the symmetry of the face. Dentoalveolar infections may involve facial spaces and cause swelling of the affected side. Trauma, ankylosis or growth retardation of the condyle also leads to facial asymmetry.

- Temporomandibular joint: Th temporomandibular (TM) joint is assessed by inspection, palpation and auscultation ofthe joint region.
- Inspection: On inspection, the mouth opening may be restricted or deviated in case of a TM joint problem. Tenderness in the joint region is also observed on mouth opening. Injury to the TM joint, during forceps delivery, can lead to bilateral bony ankylosis thereby resulting in restriction of the jaw opening. The restriction is proportional to the degree of ankylosis unilateral fibrous ankylosis causes deviation during jaw opening. The deviation is towards the side of the lesion, that is, the affected side. Deviation and restriction may be associated with tenderness over the joint(s) region.
- Palpation: Th condyles are palpated to assess the synchronisation of their movements and tenderness on palpation. It is done by the following two methods:
- Pretragic palpation: The dentist stands in front of the patient and places the index finger in front of the tragus. The patient is directed to open the jaw. This allows the palpation of the anterior and superior surfaces of the condyle.
- Intra-auricular palpation: Th dentist stands behind the patient and places the little finger intra-auricularly. The pulp of the finger is placed anteriorly and the patient is asked to open and close the mouth repeatedly. The mouth opening revolves the condyle. The posterior and inferior surfaces of the condyle can be palpated by the finger placed inside the ear.
- Auscultation: Th joint is auscultated to identify any crepitus and clicking sounds associated with the joint movement.
- Inspection: On inspection, the mouth opening may be restricted or deviated in case of a TM joint problem. Tenderness in the joint region is also observed on mouth opening. Injury to the TM joint, during forceps delivery, can lead to bilateral bony ankylosis thereby resulting in restriction of the jaw opening. The restriction is proportional to the degree of ankylosis unilateral fibrous ankylosis causes deviation during jaw opening. The deviation is towards the side of the lesion, that is, the affected side. Deviation and restriction may be associated with tenderness over the joint(s) region.
- The shape of the head: Shape is assessed by inspecting the head. The anteroposterior dimension, extending from the frontal bone to the occipital bone, is the length of the head. The lateral extent, extending from one temporal bone to the other, is the breadth of the head. The shape of the head can be one of the following when seen from above:
- Intraoral Examination A systematic approach of examining the head and neck is important before looking into the oral cavity. In the oral cavity, the soft tissues and the oropharynx have to be assessed prior to the teeth. ‘A good diagnostician counts cavities last, not fist.’ Stanley and Lincoln
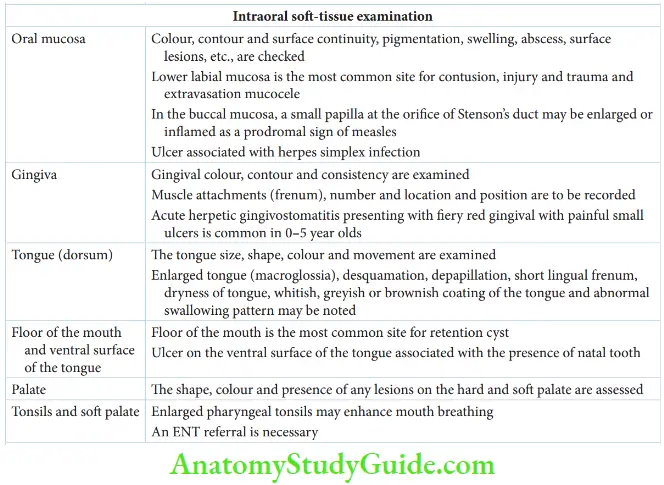
- Soft-Tissue Examination The soft tissues of the oral cavity that have to be assessed are the oral mucosae, gingiva, tongue, hard and soft palate and tonsils. The significant points to be noticed for all the tissues, especially in a paediatric patient, are as follows:
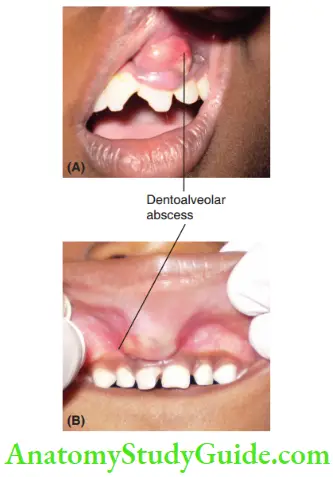
- Oral mucosa: Th colour, contour, consistency and surface continuity of the mucosae are assessed. Oral mucosa is. normally pink in colour. Melanin pigmentation can cause physiologic brownish pigmentation of the mucosa. Any swelling, abscess or mass have to be palpated with the thumb and index finger to check for consistency. Surface lesions such as ulcers, vesicles, fissures, crusts, abrasions and scars are looked for.
 1. (A) permanent central incisor and
1. (A) permanent central incisor and
2. (B) primary central incisor.- Significance Of Mucosal Examination
- Addison’s disease and intestinal polyposis may manifest as pathologic brownish or bluish-black pigmentation on the mucosae.
- Lower labial mucosa is the most common site for contusion, injury and trauma.
- Extravasation of salivary gland cysts are common in the lower lip.
- A small papilla at the orifice of Stenson’s duct may be observed in the buccal mucosa. Enlargement or inflammation of this papilla is a prodromal sign of measles.
- Ulcers associated with primary herpes simplex infection are commonly found on the attached gingiva.
- Oedematous consistency of the gingiva indicates chronic inflammatory involvement and is associated with poor oral hygiene.
- Significance Of Mucosal Examination
- Gingiva: Gingival colour, contour and consistency have to be observed. Attachment, number, location and position of the frenum have to be recorded. The maxillary arch has a single labial frenum attached in between the central incisors and usually one to three buccal frenum or free on each side between the primary fist and second molars. The mandibular arch has one labial frenum and one to three buccal frenum or free.
- Significance Of Gingival Examination Reddish, inflamed gingiva reflects poor oral hygiene associated with exfoliating teeth, erupting teeth, malposed teeth and poor motivation for oral hygiene. Draining fistulas of dentoalveolar abscesses may present as a papilla on the attached gingiva. Fiery red gingiva with painful small ulcers associated with loss of appetite, high fever and dehydration suggests acute herpetic gingivostomatitis. Primary herpes simplex infection is the commonest infection in children between the age group of 0–5 years.
- Tongue (Dorsum): Th tongue size, shape and colour are examined. The movement of the tongue has to be assessed to identify the swallowing pattern. An abnormal swallowing pattern may lead to malocclusion.
- Significance Of Tongue Examination
- An enlarged tongue (macroglossia) may be due to cretinism, Down’s syndrome or in association with a cyst or a neoplasm.
- Desquamation and depopulation of the dorsum of the tongue may be associated with avitaminosis, anaemia, stress and the chronic use of antibiotics.
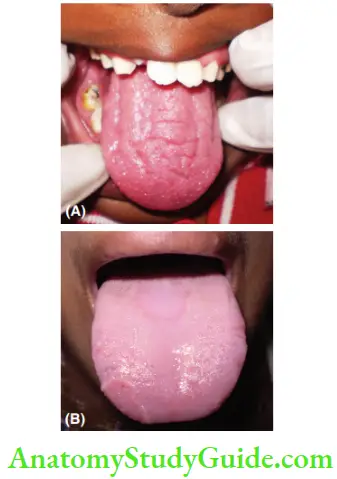
- Short lingual frenum or tongue tie may be manifested as forking at the tip of the tongue on protrusion. It may cause mispronunciation of linguoalveolar stops, linguodental fricatives and sibilants. Dryness of the tongue may be associated with dehydration and mouth breathing.
- Whitish, greyish or brownish coating of the tongue may be observed in febrile children and in the early stages of exanthematous diseases.
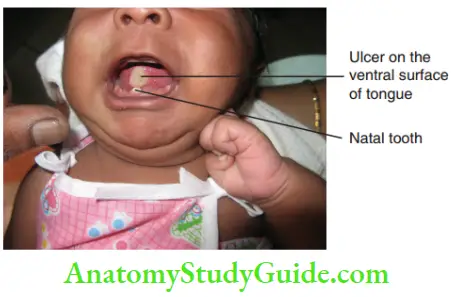
- The floor of the mouth and ventral surface of the tongue: Th floor of the mouth is the most common site for retention cysts. Swelling and ulceration in the floor of the mouth may elevate the tongue and affect speech and tongue movements. Ulcers are commonly found in the ventral surface of the tongue in the presence of a natal tooth.
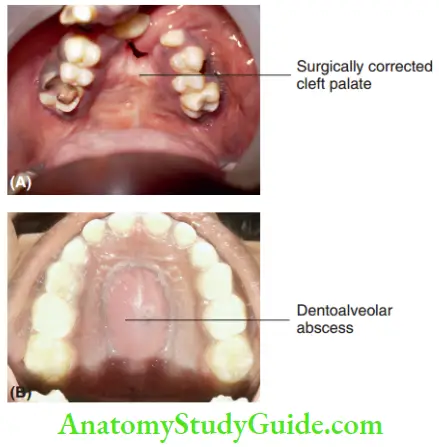
- Palate: Th child’s head is extended for direct observation of the palate. The shape, colour and presence of any lesions on the hard and soft palate are observed. The lesions may be scars of traumatic origin or scars due to surgical repair of developmental anomalies. Colour change of the palate may be due to infection, systemic diseases and chemical agents.
- Tonsils and soft palate: Th tongue is depressed with a depressor or mouth mirror to examine the tonsils and soft palate. Enlarged palatine tonsils may be a distinct septic focus in the body. Enlarged pharyngeal tonsils may contribute to mouth breathing. Referral to an ENT specialist is necessary in both conditions.
- Oral mucosa: Th colour, contour, consistency and surface continuity of the mucosae are assessed. Oral mucosa is. normally pink in colour. Melanin pigmentation can cause physiologic brownish pigmentation of the mucosa. Any swelling, abscess or mass have to be palpated with the thumb and index finger to check for consistency. Surface lesions such as ulcers, vesicles, fissures, crusts, abrasions and scars are looked for.
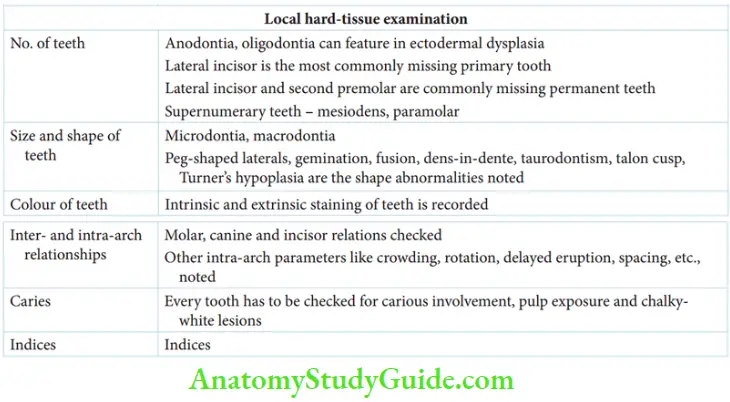
- Hard-Tissue Examination The number, size, colour, inter-arch and intra-arch relations, carious involvement and malformations of the teeth are assessed.
- A number of teeth: Primary dentition comprises five primary teeth in each quadrant and in total 20 teeth.
- Significance
- The complete absence of teeth is described as anodontia. If more than 14 teeth are absent, the condition is called oligodontia. Anodontia or oligodontia are features of hereditary ectodermal dysplasia.
- The most commonly missing tooth in primary dentition is the lateral incisor. In permanent dentition, exclusive of third molars, mandibular second premolars and lateral incisors are commonly missing.
- Fusion of primary incisors causes a decrease in the number of teeth.
- Among extra teeth or supernumerary teeth, the most common is the mesiodens which is found in the midline between the right and left central incisors. Fusion of a supernumerary tooth with a primary tooth results in an extra tooth with no increase in number.
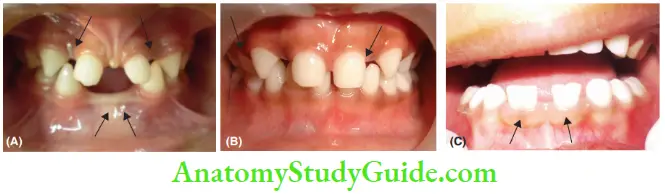
1. (A) Multiple missing primary teeth.
2. (B) Missing primary lateral incisors.
3. (C) Fusion of primary incisors.
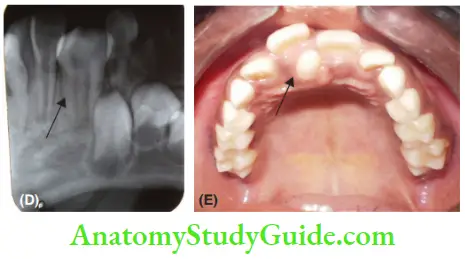
4. (D) Gemination of primary canine – two root canals are evident.
5. (E) Mesiodens. - Parapremolars and paramours are the next most common supernumerary teeth. These are called supplemental teeth owing to their resemblance to premolars and molars, respectively.
- Significance
- Size of teeth: Microdontia and macrodontia are the most common size alterations of permanent teeth. Microdontia indicates teeth size smaller than the normal teeth and macrodontia indicates teeth size larger than the normal teeth. The primary tooth most prone to size and shape alterations is the maxillary lateral incisor.
- The shape of teeth: Th teeth can show various shapes as in the case of peg-shaped lateral incisors and screwdriver-shaped incisors. The tooth malformations that result in the change of shape and/or size of the tooth also include gemination, fusion, notching of teeth, dens-in-dente, talon cusp, dens evaginates, taurodontism and Turner’s hypoplasia. Turner’s hypoplasia is a local alteration in shape/size/colour on permanent teeth due to pulpal involvement or trauma to the primary predecessor. It is observed more commonly on maxillary incisors.

6. (F) Peg-shaped incisors in an ectodermal dysplastic child.
7. (G) Talon cusp. - Colour of teeth: Primary teeth are milk-white in colour. The colour may be altered due to extrinsic or intrinsic staining. Extrinsic stains mechanically adhere on to the tooth surface and may be removed by oral prophylaxis. Chromogenic bacteria, material alba, calculus and poor oral hygiene cause extrinsic staining of teeth. Intrinsic stains are associated with altered dentin and/or enamel. Erythroblastosis foetal, blood dyscrasias, dentinogenesis imperfecta, Pamela genesis imperfect, tetracycline stains, internal resorption and devitalised pulp are common causes of intrinsic staining of teeth.
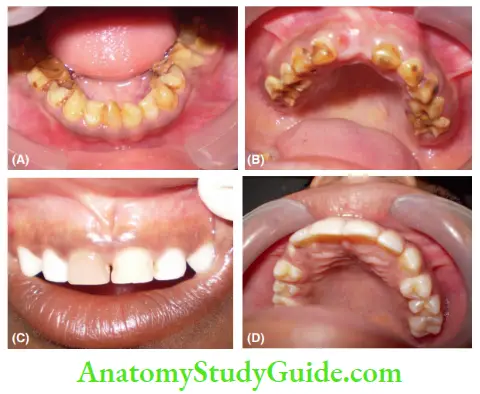 1. (A, B) Amelogenesis imperfecta.
1. (A, B) Amelogenesis imperfecta.
2. (C) Non-vital incisor.
3. (D) Extrinsic stains on the palatal surface of maxillary
incisors. - Inter-arch and intra-arch relations: Th following parameters are assessed for inter-arch and intra-arch relationships.
- Inter-arch relationship
- Primary molar relation – Flush terminal plane/mesial step/distal step
- Permanent molar relation – Angle’s Class I/Class II/Class III
- Primary canine relation – Class I/Class II/ Class III
- Permanent canine relation – Class I/Class II/ Class III
- Incisor relation – Class I/Class II/Class III
- Overjet and overbite of incisors
- Intra-arch parameters such as crowding or overlapping of teeth, spacing between teeth, rotations, malpositions and delayed eruption are noted. All the inter-arch and intra-arch parameters are discussed, in Paediatric Orthodontics.
- Inter-arch relationship
- Carious involvement: Everycarious lesion has to be excavated and assessed for possible pulp exposure. Carious lesions must not be probed as probing can cavitate the non-cavitated carious lesions and cause pulpal entry into teeth. Chalky white lesions (non-cavitated early dental decay): Chalky white lesions on teeth can either be initial demineralisation of dental caries or be enamel hypoplasia. To differentiate, the tooth surface is dried and the spot is observed. The spot is more evident when dry and disappears when wet, it is enamel demineralisation due to dental caries. If it persists on wetting, it is a hypoplastic spot.
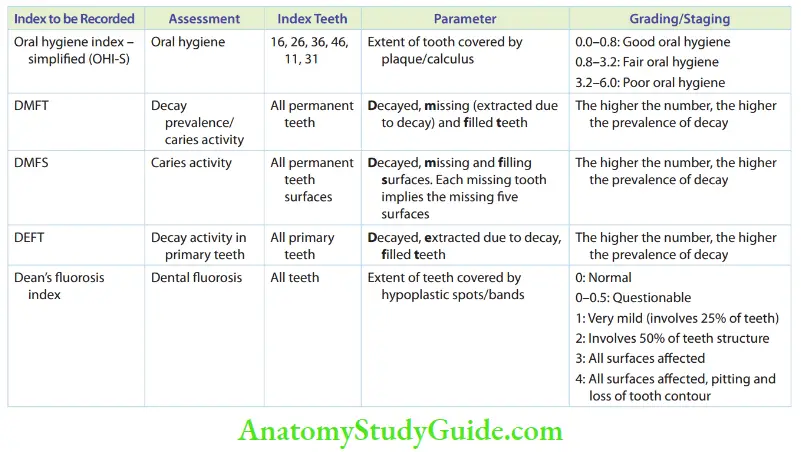
- Indices: The basic indices to be recorded in children are indices concerned with oral hygiene, caries activity and fluorosis.
- The oral hygiene index simplified (OHI-S) proposed by Green and Vermillion
- DMFT and DMFS by H Klein, Carol E Palmer and Knutson
- DEFT by Grubble
- Dean’s fluorosis index/WHO index for fluorosis
- A number of teeth: Primary dentition comprises five primary teeth in each quadrant and in total 20 teeth.
These indices are listed in Table
Summary
- The following things are to be examined as a part of the general examination:
- Local examination and associated dental findings are summarised below
Leave a Reply