Hemodynamic Disorders
Question 1. Define and classify edema. Discuss etiopathogenesis and pathology of various types of edema with examples.
Answer:
- Edema is defined as an abnormal increase in interstitial fluid within tissues. Edema fluid can be transudate or exudate
- Transudate protein-poor fluid due to increased hydrostatic pressure or reduced
- plasma proteins, for example, heart failure, renal failure, hepatic failure, malnutrition
- Transudative effusions are usually translucent and straw-colored
- Exudate inflammatory edema (protein-rich fluid that occurs as a result of increased vascular permeability)
- Exudative effusions are often cloudy due to the presence of white cells
Read and Learn More Preparatory Manual of Pathology Question and Answers
Etiopathogenesis of edema
- Increased hydrostatic pressure
- Reduced plasma osmotic pressure
- Lymphatic obstruction
- Sodium retention
- Inflammation
Pathology of various types of edema
1. Increased hydrostatic pressure can be due to:
- Impaired venous return: Congestive heart failure, constrictive pericarditis, ascites (liver cirrhosis), venous obstruction or compression, thrombosis, external pressure (example mass), lower extremity inactivity with prolonged dependency
- Arteriolar dilation: Heat, neurohumoral dysregulation
2. Reduced plasma osmotic pressure (hypoproteinemia) can be due to:
Protein-losing glomerulopathy (nephrotic syndrome), liver cirrhosis (ascites), malnutrition, protein-losing gastrenteropathy
3. Lymphatic obstruction can be due to
- Inflammatory, neoplastic, post-surgical, post-irradiation
4. Sodium retention occurs due to
- Excessive salt intake with renal insufficiency, increased tubular reabsorption of sodium, renal hypoperfusion, increased renin-angiotensin-aldosterone secretion
5. Inflammation: Acute inflammation, chronic inflammation, angiogenesis.
Question 2. Discuss in brief, the normal mechanisms involved in hemostasis.
Answer:
A sequence of events leading to hemostasis at a site of vascular injury
1. Arteriolar vasoconstriction:
- Brought about by endothelial cell injury
- Due to stimulation and release of endothelin, which is a potent vasoconstrictor
2. Primary hemostasis—formation of the platelet plug:
- Endothelial injury exposes highly thrombogenic sub-endothelial extracellular matrix (ECM) which leads to platelet adherence and activation.
- Within minutes, the secreted products recruit additional platelets (aggregation)
to form a hemostatic plug.
3. Secondary hemostasis—deposition of fibrin:
- Tissue factor is released by endothelial cells following endothelial cell injury
- Tissue factor along with factor VII initiates the coagulation pathway and results in thrombin generation
- Thrombin cleaves fibrinogen into insoluble fibrin, creating a fibrin meshwork
- This will consolidate the initial platelet plug
4. Clot stabilization and resorption:
- After the clot is formed, clot stabilization and resorption are brought about by tissue plasminogen activator, tPA
Question 3. Define Virchow’s triad. Write in detail about the pathogenesis, morphology, and fate of thrombus.
Answer:
Virchow’s triad
Three primary abnormalities that lead to thrombus formation
- Endothelial injury
- Stasis or turbulent blood flow
- Hypercoagulability of the blood
Pathogenesis
1. Endothelial injury or dysfunction:
- Causes: Hypertension, turbulent blood flow, bacterial endotoxins, radiation injury, homocystinuria or hypercholesterolemia, cigarette smoke
- Results in platelet activation and thrombus formation in the heart and arterial
circulation
2. Alteration in normal blood flow:
- Normal blood flow is laminar (platelets and blood elements flow centrally in the vessel lumen)
- Turbulent blood flow leads to arterial and cardiac thrombosis by causing endothelial injury or dysfunction
- Hyperviscosity (seen in polycythemia vera) increases the resistance for blood to flow and results in small vessel stasis
- Deformed red cells in sickle cell anemia impede blood flow through small vessels
- Stasis is a major contributor to the development of venous thrombi
3. Hypercoagulability of blood:
Definition: Any disorder of the blood that predisposes to thrombosis
This can be due to primary (genetic) or secondary (acquired) disorders
1. Inherited (genetic) causes
- Factor V gene mutation (called Leiden mutation)
- Prothrombin gene mutation
- Elevated levels of homocysteine contribute to arterial and venous thrombosis
- Anti-thrombin III, protein C or protein S deficiency
2. Acquired causes
- Prolonged bedrest or immobilization, myocardial infarction, atrial fibrillation
- Tissue injury (surgery, fracture, and burn), cancer, prosthetic cardiac valves
- Disseminated intravascular coagulation, heparin-induced thrombocytopenia
- Anti-phospholipid antibody syndrome
Morphology of Thrombus
- Arterial or cardiac thrombi begin at the sites of turbulence or endothelial injury
- Venous thrombi occur at sites of stasis
1. Antemortem thrombi:
- Shows Lines of Zahn, which represent pale platelet and fibrin deposits alternating with darker red cell-rich layers
- Lines of Zahn signify that the thrombus has formed in the flowing blood
- Are firm and focused attached
2. Postmortem clots:
- Are gelatinous with a dark red dependent portion where red cells have settled by gravity and a yellow “chicken fat” upper portion
- Are not attached to the underlying wall
Arterial thrombi:
Most favored sites include coronary, cerebral, and femoral arteries Venous thrombosis (phlebothrombosis): Lower extremities are most commonly involved followed by upper extremities, periprostatic plexus, or the ovarian and periuterine veins
Fate of Thrombus
- Propagation: Thrombi accumulate additional platelets and fibrin
- Embolization: Thrombi dislodge and travel to other sites in the vasculature
- Dissolution: As a result of fibrinolysis, there can be rapid shrinkage of recent thrombi
- Organization and recanalization: Organized by the in-growth of endothelial cells, smooth muscle cells, and fibroblasts
Question 4. Write a short note on heparin-induced thrombocytopenia.
Answer:
- Heparin-induced thrombocytopenia (HIT) syndrome
- Occurs following the administration of unfractionated heparin
- Unfractionated heparin induces the formation of antibodies against complexes of heparin and platelet factor 4
- Binding of antibodies to platelets results in their activation, aggregation, and consumption and hence thrombocytopenia
- This leads to a prothrombotic state, even in the face of heparin administration and low platelet counts
- Low-molecular-weight heparin preparations are at lower risk to induce antibody formation
Question 5. Write a short note on antiphospholipid antibody syndrome.
Answer:
Antiphospholipid antibody syndrome (lupus anticoagulant syndrome)
- Present with recurrent thrombosis, repeated miscarriages, cardiac valve vegetations, and thrombocytopenia
- Fetal loss occurs because of antibody-mediated interference with the growth and differentiation of trophoblasts, leading to a failure of placentation
- Antibodies frequently give a false-positive serologic test for syphilis as the antigen in the standard assay is embedded in cardiolipin
Two types
- Primary antiphospholipid syndrome is the presence of a hypercoagulable state without any evidence of other autoimmune disorders
- Secondary antiphospholipid syndrome (lupus anticoagulant syndrome) individuals have an associated autoimmune disease, such as SLE
Question 6. Enumerate types of embolism. Write a note on Caisson disease.
Answer:
Types of embolism
- Pulmonary embolism
- Systemic thromboembolism
- Fat and marrow embolism
- Air embolism
- Amniotic fluid embolism
Air embolism
>100 ccs of air is required to have a clinical effect on the pulmonary circulation
Causes
- During bypass surgery
- Introduced into the cerebral circulation by neurosurgery in the “sitting position”
- During obstetric or laparoscopic procedures
- As a consequence of chest wall injury
Decompression sickness
- When individuals experience a sudden decrease in atmospheric pressure
- Seen in scuba and deep sea divers, underwater construction workers, and individuals in unpressurized aircraft in rapid ascent
- During deep-sea dive, when air is breathed at high pressure, increased amounts of gas (nitrogen) are dissolved in the blood and tissues
- When the driver ascends (depressurizes) too rapidly, nitrogen comes out of the solution in the tissues and the blood resulting in damage.
Caisson disease
A chronic form of decompression sickness
Ischemic necrosis–seen in femoral heads, tibia, and humeri due to the persistence of gas emboli in the skeletal system
Question 7. Write a short note on fat embolism.
Answer:
Fat embolism
- Occurs in 90% of individuals with severe skeletal injuries
Fat embolism syndrome
- Symptomatic patients of fat embolism
- Characterized by pulmonary insufficiency, neurologic symptoms, anemia, and thrombocytopenia
- Fatal in 5% to 15% of cases
Clinical features
- Sudden onset of tachypnea, dyspnea, and tachycardia; irritability and restlessness, 1 to 3 days after injury
- Diffuse petechial rash due to rapid onset of thrombocytopenia is a diagnostic clue
Lab findings
- Thrombocytopenia—due to the platelet adhesion to fat globules
- Anemia can result from red cell aggregation and/or hemolysis
- Paraffin embedding cannot diagnose fat as these are dissolved out of the tissue preparations by the solvents
- Frozen sections and special stains for fat are used to diagnose lipids
Question 8. Write a short note on amniotic fluid embolism.
Answer:
- A major cause of maternal mortality worldwide
- Occurs during labor and in the immediate postpartum period
Clinical features
- Sudden severe dyspnea, cyanosis, and shock followed by neurologic impairment (headache to seizures and coma)
Cause
- Infusion of amniotic fluid or fetal tissue into the maternal circulation due to a tear in placental membranes or rupture of uterine veins
Diagnosis
- Requires the presence of squamous cells shed from fetal skin, lanugo hair, mucin derived from the fetal respiratory or gastrointestinal tract in the maternal pulmonary microvasculature
Question 9. Write a short note on the morphology of an infarct.
Answer:
Infarcts can be red (hemorrhagic) or white (anemic):
Red (hemorrhagic) infarcts:
- Occurs with venous occlusions (example ovary), in loose tissues (example lung), in tissues with dual circulations (e.g. lung and small intestine)
- When the flow is re-established to a site of previous arterial occlusion and necrosis (for example, following angioplasty of an arterial obstruction)
White (anemic) infarcts
- Occurs with arterial occlusions in solid organs with end arterial circulation (for example heart, spleen, and kidney)
- Points to remember
- Infarcts are wedge-shaped
- Dominant histology of infarction is ischemic coagulative necrosis except in central nervous system infarction, which results in liquefactive necrosis
- Most of the infarcts are ultimately replaced by scar
Question 10. Define shock, enumerate types of shock, and discuss the pathogenesis and morphological changes in shock.
Answer:
Definition: Shock is defined as reduced cardiac output which impairs tissue perfusion
and leads to cellular hypoxia
Types of shock
1. Cardiogenic shock:
- Causes: Myocardial infarction, ventricular rupture, arrhythmia, cardiac tamponade, pulmonary embolism
2. Hypovolemic shock
- Causes: Massive hemorrhage or fluid loss from severe burns
3. Shock associated with systemic inflammation:
- Causes: Microbial infections, burns, trauma, and pancreatitis
4. Neurogenic shock
- Causes: Anesthetic accident or a spinal cord injury
5. Anaphylactic shock
- Causes: IgE–mediated hypersensitivity reaction
Pathogenesis of Shock
1. Inflammatory cell response
- Upon activation by the microbial products, innate immune cells produce TNF, IL-1, IFN-γ, IL-12, and IL-18 → resulting in cytokine production and endothelial activation
- Activation of complement cascade → resulting in production of anaphylatoxins(C3a C5a), chemotactic fragments (C5a) and opsonins (C3b)
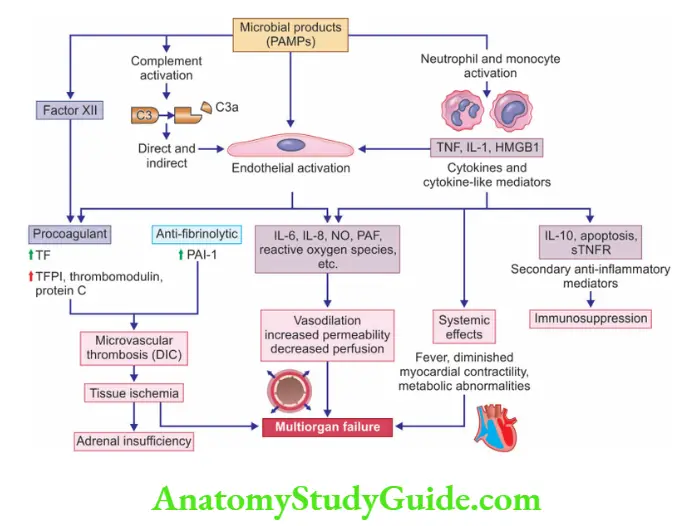
2. Endothelial activation and injury
- Activation of endothelial cells due to sepsis leads to vascular leakage and tissue edema
3. Induction of a procoagulant state
- Inflammatory cytokines favor coagulation by increasing tissue factor production by endothelial cells
- Activation of widespread coagulation factors results in disseminated intravascular Coagulation (DIC) like the picture
- In full-blown DIC, as there occurs complete utilization of coagulation factors, bleeding, and hemorrhage are likely complications
4. Metabolic abnormalities
- Sepsis patients exhibit insulin resistance and resultant hyperglycemia
5. Organ dysfunction
- Systemic hypotension and thrombosis result in tissue hypoperfusion and resultant multiorgan failure
- Morphological changes in shock
- The adrenal gland shows cortical cell lipid depletion
- Kidney shows acute tubular necrosis
- Lungs show diffuse alveolar damage or shock lung
- DIC resulting in multiple petechial hemorrhages on serosal surfaces and skin
Leave a Reply