Lower Urinary Tract and Male Genital Tract
Question 1. Write a note on the grading of urothelial tumors (seen in the urinary bladder).
Answer:
WHO/International Society of Urological Pathology (ISUP) grading of urothelial tumors
- Urothelial papilloma
- Urothelial neoplasm of low malignant potential
- Papillary urothelial carcinoma, low-grade
- Papillary urothelial carcinoma, high-grade
- Carcinoma in situ
- Invasive urothelial cancer
Read and Learn More Preparatory Manual of Pathology Question and Answers
1. Urothelial papillomas
- Small superficial exophytic structures attached to the bladder mucosa with a stalk
- Papillae have a central core of loose fibrovascular tissue covered by epithelium, which resembles normal urothelium histologically
2. Papillary urothelial neoplasms of low malignant potential (PUN LMP)
- These tumors are larger than papillomas
- Papillae with a thicker urothelial layer in comparison to papilloma
3. Low-grade papillary urothelial carcinomas, non-invasive
- Urothelial cells have an orderly architectural and cytological appearance
- Tumor cells are cohesive and show mild nuclear atypia with a few cells showing hyperchromatic nuclei and infrequent mitotic figures
4. High-grade papillary urothelial cancers, non-invasive
- Tumor cells are dyschezia with large hyperchromatic nuclei
- Atypical mitotic figures are frequent
- These tumors can show invasion into the muscular layer
5. Carcinoma in situ
- Can present as reddening, granularity, and thickening of the bladder mucosa
- Tumor cells lack cohesiveness and can be easily shed in urine
- Microscopy: It shows the presence of cytologically malignant tumor cells within a flat urothelium
6. Invasive urothelial cancer:
- Highly atypical pleomorphic tumor cells with invasion into the deeper muscular layers
- The extent of the invasion into the muscular mucosae is of prognostic significance
Question 2. Write a note on the etiopathogenesis of transitional cell carcinoma of the bladder.
Answer:
Factors implicated in the causation of bladder cancer/ transitional cell carcinoma
- Cigarette smoking
- Industrial exposure to arylamines
- Schistosoma crematorium infection
- Long-term use of analgesics
- Heavy long-term exposure to cyclophosphamide
- Pelvic irradiation for other cancers
- Genetic alterations:
- Gain of function mutations in FGFR3
- Loss of function mutations in TP53 and RB tumor suppressor genes
- Activating mutations in HRAS oncogene
- Monosomy or deletions of chromosome 9p and 9q
Question 3. Write a short note on condyloma acuminate (warts) affecting the male genital tract.
Answer:
Condyloma acuminatum
- Causative agent (sexually transmitted disease): Human papillomavirus (HPV) types 6 and 11
- The site and gross features: Most commonly affect the coronal sulcus and the inner surface of the prepuce, where they present as single or multiple, sessile or pedunculated, red papillary excrescences
Microscopy
- The lesion is composed of branching, villous, papillary connective tissue stoma, covered by the epithelium with hyperkeratosis and acanthuses (thickening of the underlying epidermis)
- Surface epithelium shows characteristic viral cytopathic change/ pilocytic Styria
- Koilocytic atypia: Manifests as nuclear enlargement, hyperchromasia, and a cytoplasmic perinuclear halo
Question 4. Write a short note on Bowen’s disease.
Answer:
Bowen disease
- Affects males more than 35 years of age
- Site: Involves the skin of the shaft of the penis and the scrotum
- Gross: Solitary, thickened, gray-white, opaque plaque
Microscopy
- Epidermis appears hyperplastic
- Cells in the stratum spinous show full-thickness epithelial dysplasia with large hyperchromatic nuclei and lack orderly maturation with numerous mitosis
- The basement membrane is intact
- Can transform into infiltrating squamous cell carcinoma
Note:
- Bowen disease of the glans is termed erythroplasia of Quart
Question 5. Write a short note on cryptorchidism.
Answer:
Cryptorchidism. Definition:
Complete or partial failure of intra-abdominal testes to descend into the scrotal sac. Undescended testis is at a greater risk of developing testicular cancer than is the descended testes
Two phases of testicular descent
1. Trans-abdominal phase
- Testis comes to lie within the lower abdomen or brim of the pelvis
- Controlled by a hormone called müllerian-inhibiting substance
2. Inguinoscrotal phase
- Testes descend through the inguinal canal into the scrotal sac
- Occurs due to the release of calcitonin gene-related peptide from the genitofemoral nerve
- The most common site of arrest is in the inguinal canal
Morphology
- Unilateral in most cases, bilateral in 25% of patients
Microscopy
- Altered morphological changes in testes appear as early as 2 years of age
- Characterized by maturation arrest of germ cells
- Tubules show only Sertoli cells
- Marked hyalinization and thickening of the basement membrane of the tubules
- Leydig cells appear prominent
Treatment
- Orchiopexy (placement in the scrotal sac) should be done preferably before 2 years of age
- Orchiopexy does not guarantee fertility and development of cancer in the testes
- Cancer may also develop in the contralateral, normally descended testis
Question 6. Classify germ cell tumors. Discuss gross and microscopic pictures of seminoma testis.
Answer:
Germ cell tumors
1. Seminomatous tumors
- Seminoma
- Spermatocytic seminoma
2. Non-seminomatous tumors
- Embryonal carcinoma
- Yolk sac (endodermal sinus) tumor
- Choriocarcinoma
3. Teratoma
4. Sex cord-stromal tumors
- Leydig cell tumor
- Sertoli cell tumor
Seminole
- The most common type of germ cell tumor
- Seen most commonly in the third decade
- The ovarian counterpart of Seminole is dysgerminoma
- Contains ISO-chromosome 12p
- Expresses OCT3/4 and NANOG
- 25% of these tumors have activating KIT mutations
Morphology
Gross
- Produce bulky masses
- Cut surface: Appears homogeneous, gray-white, lobulated
- Hemorrhage or necrosis is not seen
Microscopy
- The tumor is composed of sheets of uniform tumor cells
- Tumor cells are divided into poorly demarcated lobules by delicate fibrous septa
- The fibrous septae contain lymphocytic infiltrate
- Tumor cells are large, round to polyhedral, have distinct cell membranes; clear or watery-appearing cytoplasm, a large, central nucleus with one or two prominent nucleoli
Question 7. Write a short note on spermatocyte seminoma.
Answer:
Spermatocytic seminoma
- Slow growing tumor
- Affects individuals older than age 65 years
- Excellent prognosis
- Gross: Soft, gelatinous appearance
Microscopy
Three cell populations
- Medium-sized cells (most numerous) containing a round nucleus and eosinophilic cytoplasm with a characteristic spire chromatin (which resembles that of spermatocytes in the meiotic phase)
- Smaller cells resembling small lymphocytes
- Scattered giant cells, either uninucleate or multinucleate
Question 8. Write a note on the pathogenesis and morphology of benign prostatic hypertrophy.
Answer:
Benign prostatic hyperplasia (BPH)
Etiopathogenesis
- Hyperplasia occurs due to impaired cell death rather than increased epithelial cell proliferation
- Androgens required for the development of BPH, increase cellular proliferation and inhibit cell death
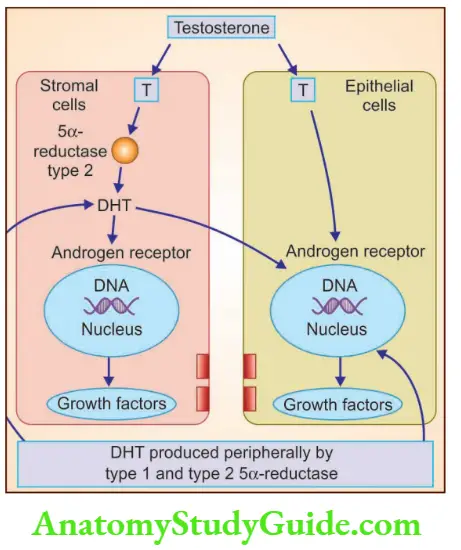
- Dihydrotestosterone (DHT) is the major androgen in the prostate
- DHT is formed in the prostate from testosterone by the action of an enzyme called type 2 5α-reductase
- This enzyme is located in stromal cells
- Hence, stromal cells are responsible for androgen-dependent prostatic growth
- DHT binds to the nuclear androgen receptors (AR) present in both stromal and epithelial prostate cells
- DHT is more potent than testosterone because it has a higher affinity for AR
- The binding of DHT to AR stimulates the transcription of androgen-dependent genes, which includes several growth factors and their receptors
- DHT-induced growth factors act by increasing the proliferation of stromal cells and decreasing the epithelial cell death
Question 9. Write a short note on prostatic intraepithelial neoplasm.
Answer:
Prostatic intraepithelial neoplasm (PIN)
- Also called prostatic carcinoma in situ
- Involves prostatic ducts and acini
- Divided into three grades: PIN I, II, III
- Categories: PIN I and PIN II—low grade, PIN III—high grade
- Morphological differentiation between low grade and high grade is based on: Cell crowding and stratification; nuclear enlargement, pleomorphism, and chromatin pattern; and appearance of nucleoli
- High-grade PIN has an association with prostatic adenocarcinoma
Leave a Reply