Periodontopathy In Children Introduction
Gingivitis and gingival enlargement are very common in children. On the contrary, the prevalence of periodontitis is extremely rare in children. Loss of periodontal attachment implies that the periodontium is involved. Slowly progressing gingivitis developing into periodontitis has not been demonstrated at large in primary and mixed dentition. The explanation for uncommon involvement is quite ambiguous yet.
Table of Contents
The absence of col in primary dentition may be a significant reason. The immune mechanisms (defence mechanisms against periodontal pathogens) of the periodontium in primary and permanent teeth are reported to be distinctly different.
Read And Learn More: Paediatric Dentistry Notes
Defence mechanisms in permanent dentition involve several inflammatory mediators that induce the loss of periodontal supporting structures. These mediators are significantly less in the primary dentition. This may be the most probable cause of periodontitis being extremely rare in primary dentition.
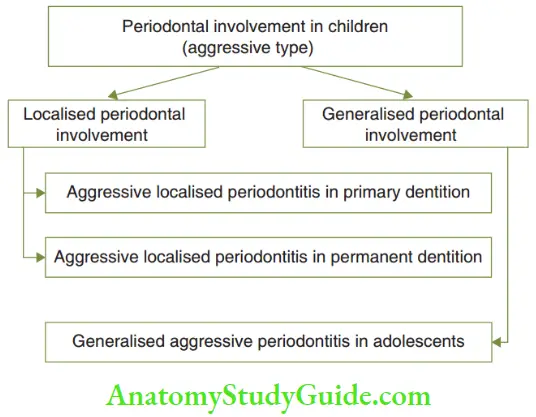
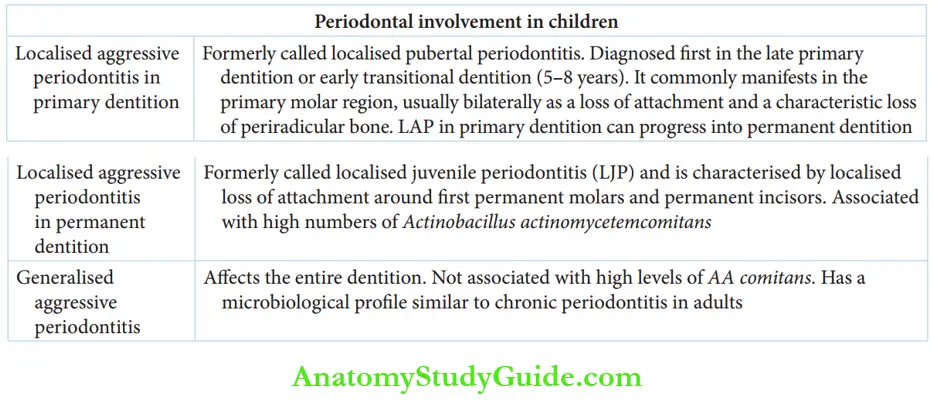
Aggressively progressing periodontitis, although rare, can involve children and adolescents. It may be a manifestation of an underlying systemic disease. Various types of periodontal involvement in children are depicted in Figure.
Localised Aggressive Periodontitis
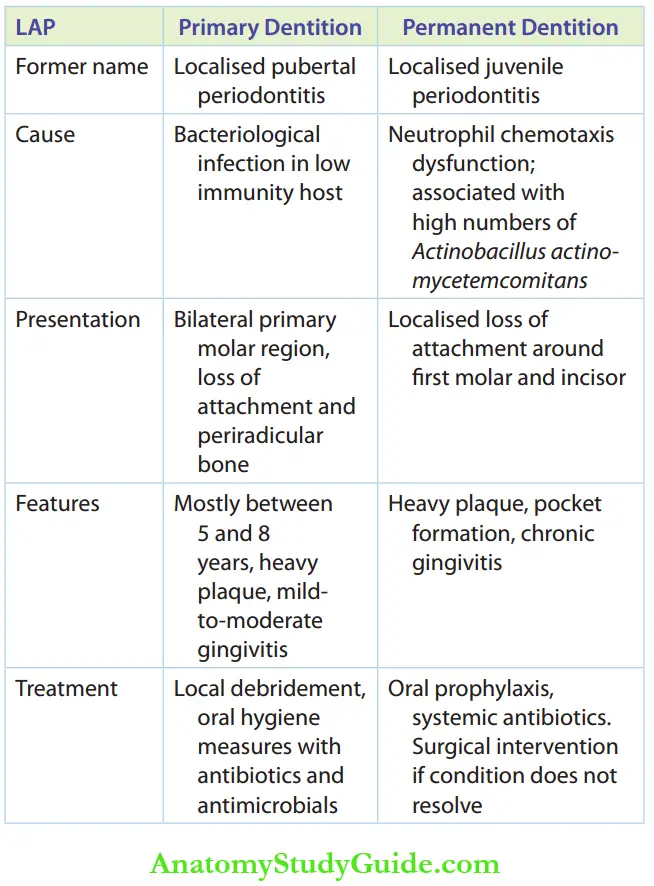
Localised aggressive periodontitis (LAP) may affect the primary dentition and permanent dentition. It was formerly called localised pubertal periodontitis. When the permanent dentition was affected, the condition was formerly called localised juvenile periodontitis.
Researchers believe that LAP in permanent and primary dentition is a single entity. LAP in primary dentition can progress into permanent dentition, differing only in the age of onset or timing of diagnosis.
- Lap In Primary Dentition LAP in primary dentition is proposed to be a bacteriological infection superimposed on subjects with a bacteriological infection superimposed on hosts with immunological defects. It is diagnosed first in the late primary dentition or early transitional dentition (5–8 years). It commonly manifests in the primary molar region, usually bilaterally, as a loss of attachment and a characteristic loss of periarticular bone. It is associated with heavier plaque and mild-to-moderate gingival inflammation with or without calculus. Local debridement and adept oral hygiene measures with antibiotics such as doxycycline and antimicrobials such as metronidazole are the treatment modes. The figure shows a typical case of localised aggressive periodontitis before and after treatment. The OPG shows loss of periarticular bone. A clinical picture of hyperkeratosis of hands and feet is depicted. Periodontitis with palmoplantar hyperkeratosis is better described as Papillon–Lefèvre syndrome.
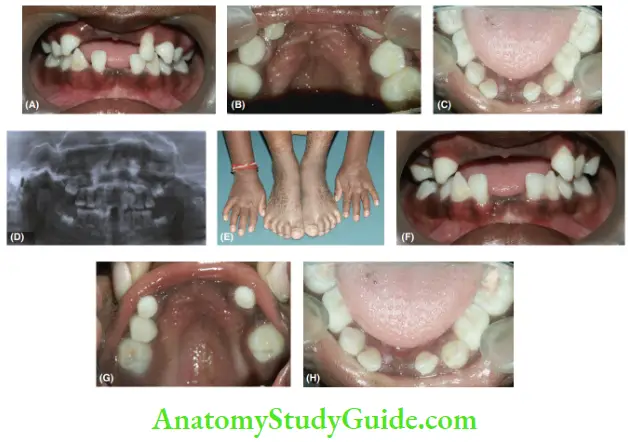
1. (A–C) Pre-operative pictures showing gingivitis and heavy plaque accumulation.
2. (D) OPG showing periradicular bone loss.
3. (E) Hyperkeratosis of palms, hands and feet.
4. (F–H) Post-operative pictures showing healing, uninflamed gingiva. - Lap In Permanent Dentition LAP in permanent dentition has been found to be associated with a neutrophil chemotaxis dysfunction and this trait is inherited by an autosomal dominant pattern. It is also found to be associated with high numbers of Actinobacillus actinomycetemcomitans (AA comtans). LAP is characterised by localised loss of attachment around the first permanent molars and permanent incisors. The amount of plaque will be greater than the one associated with chronic gingivitis and the rate of progression of attachment loss (pocket formation) is also quicker. The treatment objective is to eradicate AA comitans. Oral prophylaxis to establish good oral hygiene is the basic treatment mode. Systemic tetracyclines, metronidazole (5 mg/kg body weight, 8 hourly) with amoxicillin (20–40 mg/kg, t.i.d.) are effective systemic antibiotic regimes to arrest disease progression. Reattachment and resolution of periodontal defects can occur after the eradication of AA comitans. Localised surgical intervention may be necessary if periodontal defects do not resolve. Table compares the aetiology, clinical features and treatment methods of localised aggressive periodontitis in primary and permanent dentition.
Generalised Aggressive Periodontitis
Generalised aggressive periodontitis (GAP) occurs in adolescents and teenagers and differs from LAP in the following aspects:
- It affects the entire dentition.
- It is not associated with high levels of AA comitans.
- It has a microbiological profile similar to chronic periodontitis in adults.
The treatment mode consists of oral prophylaxis, maintenance of good oral hygiene and systemic antibiotic therapy. A microbial assay can be done to spot the dominant bacteria.
Periodontitis In Systemic Diseases
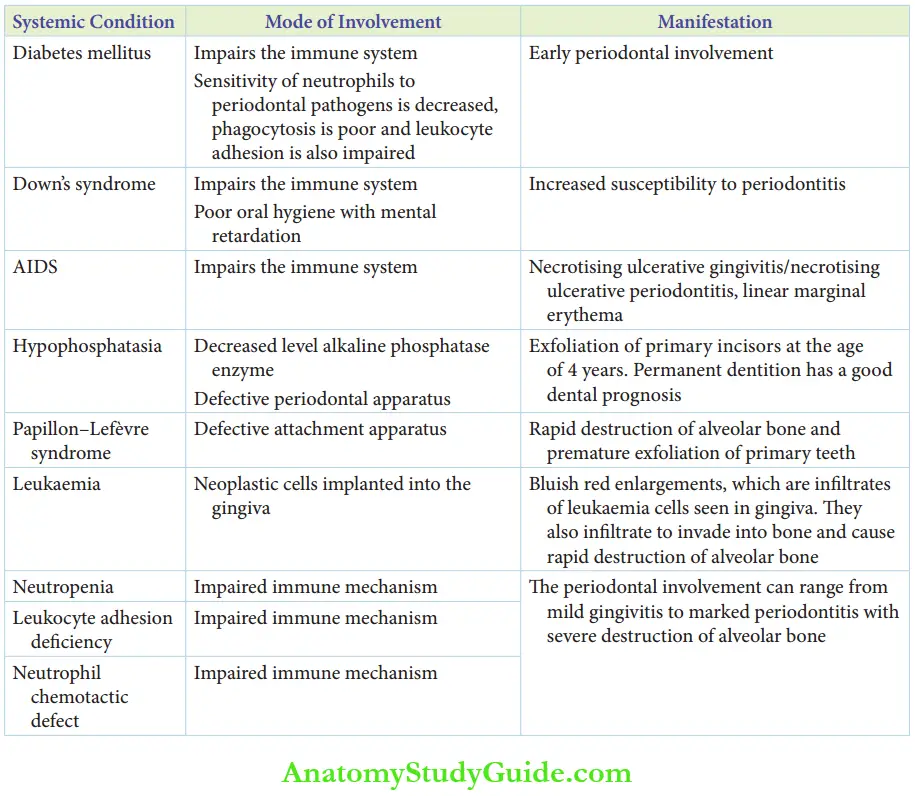
Loss of periodontal attachment or periodontitis can be observed as an intraoral manifestation in certain systemic conditions. The systemic condition can affect the periodontium in the following three ways:
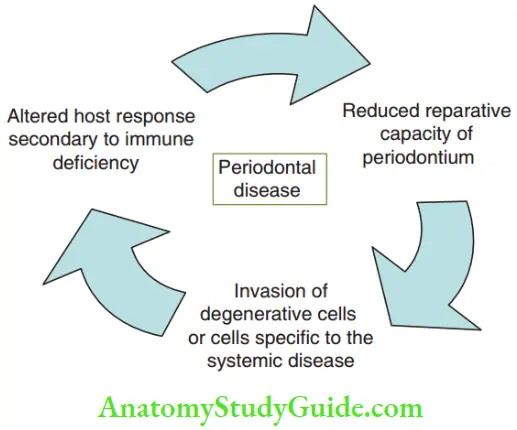
- The immune system of the child may be defective, thus altering the host response to periodontal microorganisms (for example leucocyte adhesion deficiency, neutrophil chemotactic defect, neutropenia, AIDS and Down’s syndrome)
- Reduced reparative capacity leading to defective periodontal attachment apparatus that may be prone to degradation/deterioration (for example hypophosphatasia and diabetes mellitus)
- Invasion of neoplastic cells into the attached gingiva (for example leukaemia)
The common systemic conditions that involve periodontium in children are as follows:
- Diabetes mellitus
- Down’s syndrome
- AIDS
- Hypophosphatasia
- Papillon–Lefèvre syndrome
- Leukaemia
- Neutropenia
- Leukocyte adhesion deficiency
- Neutrophil chemotactic defect
- Diabetes Mellitus Diabetes mellitus is a metabolic disorder involving an increase in blood glucose due to a deficiency of insulin (insulin-dependent, type 1) or poor peripheral utilisation of glucose (non-insulin-dependent, type 2). Insulin-dependent diabetes is more common in children. The manifestations are decreased sensitivity of neutrophils to periodontal pathogens, poor phagocytosis and impaired leukocyte adhesion. These factors alter host immunity and make the periodontium prone to degradation. 10%–15% of teenagers with insulin-dependent diabetes have demonstrated significant periodontal involvement. Poor metabolic control of the systemic condition worsens periodontal involvement.
- Treatment When the diabetic status is under vigilant control, no significant fidings are demonstrated in the gingiva. When uncontrolled, exuberant gingival involvement quite disproportionate to the number of local factors is noted. The gingival involvement ranges from enlargement to exudation. Treatment approaches include medical intervention by the paediatric physician to control the systemic condition and dental intervention. The dentist considers oral prophylaxis and subgingival scaling/curettage (where required) for the maintenance of good oral hygiene and periodical reviews.
- Down’S Syndrome Down’s syndrome is a genetic disorder involving trisomy of chromosome 21. It is associated with an increased susceptibility to periodontitis due to the following reasons:
- Demonstrable leukocyte dysfunction
- High amount of local factors due to the patient’s inability to maintain good oral hygiene independently
- High frenal attachment and gingival recession, commonly in the mandibular anterior region
- Macroglossia (a feature of the syndrome) leading to protrusion of teeth and malocclusion, predisposing to periodontal disease
- Treatment The treatment modalities involve an assessment of immune response by a paediatric physician, oral prophylaxis and motivation of the child/ caretaker to maintain good oral hygiene, followed by periodic assessment of the periodontal condition.
- Aids Acquired immunodeficiency syndrome is caused by human retrovirus that affects the B cell-mediated humoral immunity. Viral infection, malnutrition, stress and lack of sleep are predisposing factors for the oral manifestations of AIDS. Necrotising ulcerative gingivitis/necrotising ulcerative periodontitis (NUP/NUG) and linear gingival erythema are characteristic intraoral manifestations of AIDS. Necrotising ulcerative gingivitis is a rapid onset of painful gingivitis, marginal necrosis and ulceration. Microbiological assay demonstrates a high level of spirochetes and Prevotella intermedia. NUG with loss of periodontal attachment with severe bone loss and deep pockets is described as necrotising ulcerative periodontitis (NUP). Oral prophylaxis and maintenance of good oral hygiene can rapidly resolve the disease. Systemic antibiotic therapy is required only when an elevated body temperature is associated. Linear marginal erythema is characterised by an asymptomatic, reddish gingival margin of 3 mm. It signifies the endothelial degeneration of the terminal gingival capillaries. Current research also suggests that the linear gingival erythema is a candidal infection.
- Hypophosphatasia is a genetic disorder involving a decreased level of the alkaline phosphatase enzyme. This enzyme is responsible for bone deposition and mineralisation of dental tissues. The disease causes premature exfoliation of primary incisors, by 4 years. The earlier the disease manifests, the more severe it is. The early loss of teeth is due to defective cementum formation, hence poor attachment of the tooth to bone. The earlier a primary tooth erupts, the more it can be involved. The prognosis is fair when permanent teeth are affected. Hypophosphatasia is diagnosed with a decreased level of alkaline phosphatase in serum and is managed by a paediatric physician. However, there are no treatment modes with proven efficacy for the disease. Good oral hygiene can be established and the child can be motivated to upkeep the same.
- Papillon–Lefèvre Syndrome Papillon–Lefèvre syndrome is a rare genetic disorder characterised by hyperkeratosis of palms and soles, calcification of the cerebrum and early onset of aggressive periodontal involvement. The onset of periodontitis is in the primary or transitional dentition. The age of onset is around 5 years but can occur earlier too. The periodontitis persists to involve permanent dentition. The periodontitis manifests as rapid destruction of alveolar bone and premature exfoliation of primary teeth. Therapy includes aggressive modes of plaque control with systemic antibiotics such as doxycycline.
- Leukaemia Leukaemia is a haematological neoplasm characterised by an abnormal increase in immature white blood cells. It can be acute or chronic and lymphocytic and myeloid. 75% of leukemic adults have been reported to have oral manifestations as compared to 29% in leukemic children. Acute lymphocytic leukaemia (ALL) is the most common type in children followed by acute monocytic leukaemia (AML) and the juvenile type of chronic monocytic leukaemia (CML). Oral manifestations of leukaemia in children are petechiae and ecchymoses of the mucous membrane, gingival bleeding, gingival hypertrophy and nonspecific ulcerations. Regional lymphadenopathy is also common. Of the oral manifestations, petechiae, ecchymoses and bleeding are common in ALL. Gingival enlargement is common in AML. Bluish red foci of enlargements are noted in the gingiva. These enlargements are infiltrates of leukaemia cells. The infiltrates can also invade into the bone and cause rapid destruction of the alveolar bone. The therapy is planned with the paediatric physician on his assessment of the magnitude of the disease. Oral prophylaxis and plaque control are primary. Excision of the enlargement can be done on remission of the leukemic status.
- Immune-Compromised States A defect in the host immune mechanism to counter the activity of periodontal microbiota can be caused in conditions such as leukocyte adhesion dysfunction and neutropenia. A defect in neutrophil chemotaxis is also found in juvenile periodontitis
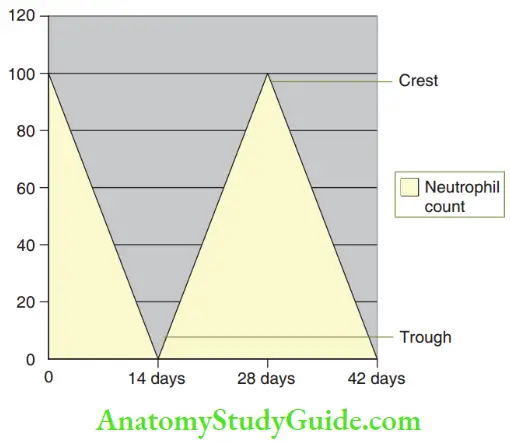
- Neutropenia is characterised by a reduction or complete disappearance of polymorph neutrophils (PMNs) that increase the susceptibility of the individual to acute infections including periodontitis. The periodontal involvement can range from mild gingivitis to marked periodontitis with severe destruction of the alveolar bone. Neutropenia can also occur in a cyclical pattern. The condition is described as cyclic neutropenia. The cyclical pattern involves a 14-day course where the number of neutrophils drops to a near-zero value (trough) every 14 days and rises to an almost normal count at the end of the cycle (crest). Lesions are more pronounced at the troughs of the neutrophil count of the cycle and less pronounced at the crests of the cycle. Therapy involves medical intervention by the paediatric physician and maintenance of oral hygiene by prophylaxis.
- Leukocyte Adhesion Deficiency (LAD) LAD is a rare genetic disorder where the protein CD 18 is defective or absent on the surface of the leukocytes. This leads to poor chemotaxis and impaired phagocytosis and predisposes the affected individual to infections including periodontitis. Medical intervention is focused to control systemic pathology. Good oral hygiene maintenance can induce remission of the oral manifestations of this disease.
Summary
- Periodontal involvement is rare in children. This may be due to the absence of col and significantly fewer inflammatory mediators in the primary dentition.
- Aggressive periodontitis although rare, can occur in children and adolescents.
Leave a Reply