Endodontic Treatment Of Young Permanent Teeth Introduction
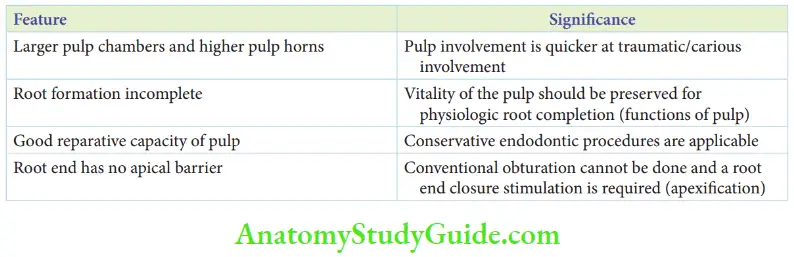
A permanent tooth that has recently erupted into the oral cavity can be described as young and immature. This is because its root formation is incomplete. The anatomical features of such a tooth involve unique modes of treatment. The significance of the young permanent teeth is as follows:
Table of Contents
- The pulp chamber is large and pulp horns are higher as pulp regression has not surfaced. Hence, the tooth is prone to pulpal involvement due to trauma, and the carious lesion spreads quicker.
- Root formation is incomplete and the apex is rightly described as a ‘blunderbuss’. The vitality of pulp should be preserved and retained for physiologic root completion (function of pulp).
- Higher vascularity and a higher proportion of undifferentiated mesenchymal cells in pulp denote good reparative capacity in case of reversible inflammation due to insult or injury. Hence, conservative endodontic procedures are indicated.
- Gutta-percha obturation is done in conventional root canal treatment of permanent teeth. But it is impractical in newly erupted permanent teeth as the canal apex is blunderbuss with no apical barrier for gutta-percha obturation. When gutta-percha obturation is attempted, obturation beyond the apex is possible. Hence, the root end closure should be stimulated before obturation.
Read And Learn More: Paediatric Dentistry Notes
The various endodontic treatment procedures performed on young permanent teeth are as follows:
- Indirect pulp capping
- Direct pulp capping
- Apexogenesis
- Apexification
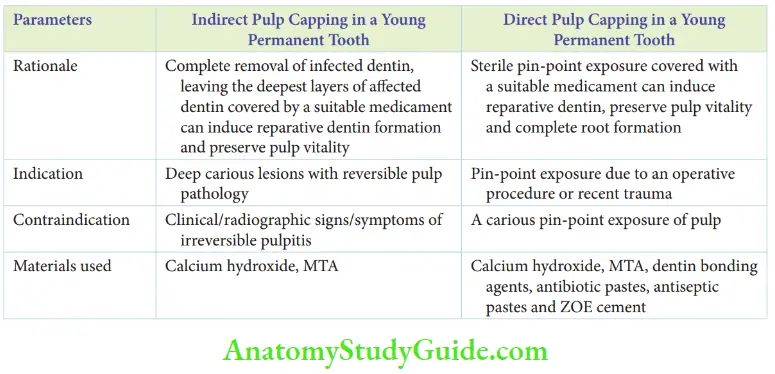
Indirect Pulp Capping
Indirect pulp capping (IPC) is a mode of managing deep carious lesions with reversible pulpal injury. It is also performed on teeth in which complete excavation of caries can expose the pulp. The differences between IPC on young permanent teeth and that on primary teeth are as follows:
- Calcium hydroxide cement preparation is contraindicated in primary teeth but it is the material of choice in permanent teeth
- The procedure on primary teeth does not require a re-entry. IPC on permanent teeth requires re-entry after 6 -8 weeks. In this re-entry procedure, the leftover carious dentin is removed and the final permanent restoration is done.
-
- Procedure Th procedure involves the complete removal of the infected dentin and the mineral is able to affect dentin from the walls of the cavity.
- The affected dentin is left on the floor of the cavity. A suitable medicament is placed to induce postmitotic odontoblasts to regulate their secretory activities and secret tertiary dentin.
- It also helps odontoblasts to differentiate from undifferentiated mesenchymal cells.
- The th cavity is filled with intermediate restorative material (IRM) and a stainless steel crown is fitted on the tooth. The restoration is re-entered after 6 -8 weeks.
- The medicament and the deepest layers of infected caries are removed. The affected dentin may be left behind.
- Calcium hydroxide or a glass ionomer lining is applied and the tooth is restored with glass ionomer cement.
- The stainless steel crown is luted back in place. This can be replaced with a permanent crown when the child is 17 years old.
Direct Pulp Capping
Direct pulp capping procedure is indicated in case of a small, pin-point exposure of the pulp. The procedure is limited to permanent teeth and is highly successful in the same.
- Indications And Contraindications Direct pulp capping is indicated in case of a sterile pin-point exposure of the pulp during an operative dentistry procedure under rubber dam isolation.
- It is indicated in pin-point exposure of the pulp due to a clean fracture (unclad by debris/any foreign material) from a recently sustained trauma.
- The procedure is contraindicated in a carious pin-point exposure as the pioneer bacteria can be demonstrated in the deeper layers.
- In this case, cariogenic pathogens and their bacterial products can possibly dissipate into the pulp and initiate an irreversible, inflammatory process.
- A pulpectomy is the treatment of choice in such situations.
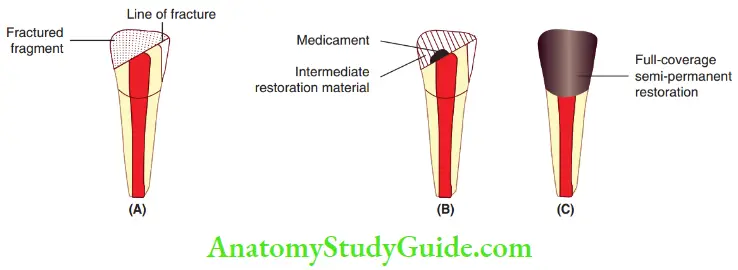
1. (A) Indicated in an accidental pulp exposure due to a clean fracture.
2. (B) It involves placement of a suitable medicament over pulp on the attainment of haemostasis.
3. (C) It requires a full-coverage restoration.
- Rationale The objective of direct pulp capping is to ‘spur’ the differentiation of odontoblasts to secrete dentin and ultimately preserve the vitality of the pulp. At the site of pulpal exposure, odontoblasts are lost. The medicament in contact with the pulp can initiate undifferentiated mesenchymal cells to differentiate into odontoblasts. These odontoblasts can secrete the dentinal matrix.
- Medicament Calcium hydroxide and mineral trioxide aggregate (MTA) are the most commonly used materials. The other medicaments that can be used for direct pulp capping are as follows:
- Calcium hydroxide with MTA
- Antibiotic paste
- Dentin bonding agents such as 4-META
- Anti-inflammatory pastes
- Antiseptic pastes
- Zinc oxide eugenol
- Procedure Th site of pin-point exposure of pulp, under the rubber dam isolation, is irrigated with saline. Pressure is applied by a small cotton pellet moistened with saline for a few minutes. This controls the bleeding. If the bleeding persists, the tooth is indicated for pulpotomy or pulpectomy. The medicament (a mix of calcium hydroxide cement and MTA) is placed over the exposure site. The medicament should not be kept on the bleeding pulp or a blood clot. A thick mix of zinc oxide eugenol or IRM is placed over the medicament. A full restoration or a full-coverage restoration is placed over the treated tooth. The young permanent tooth treated with direct pulp capping does not require a re-entry. The medicament is expected to initiate the differentiation of odontoblasts from undifferentiated mesenchyme to form reparative dentin.
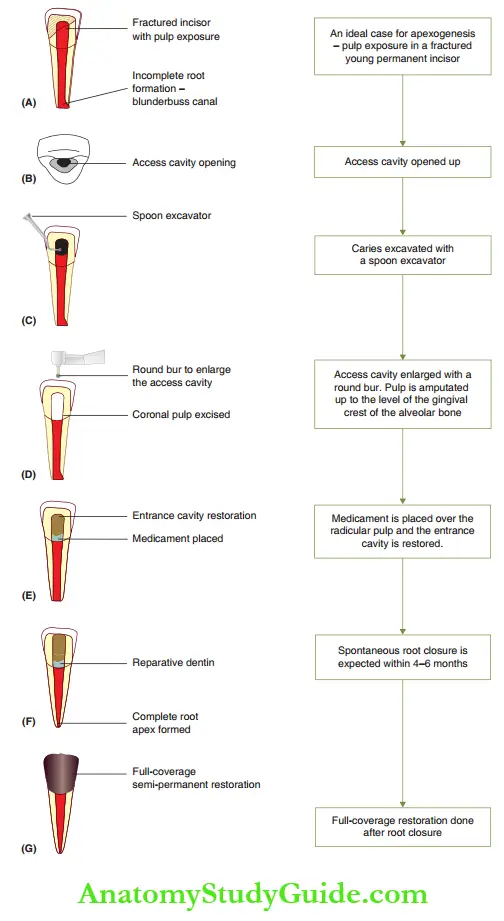
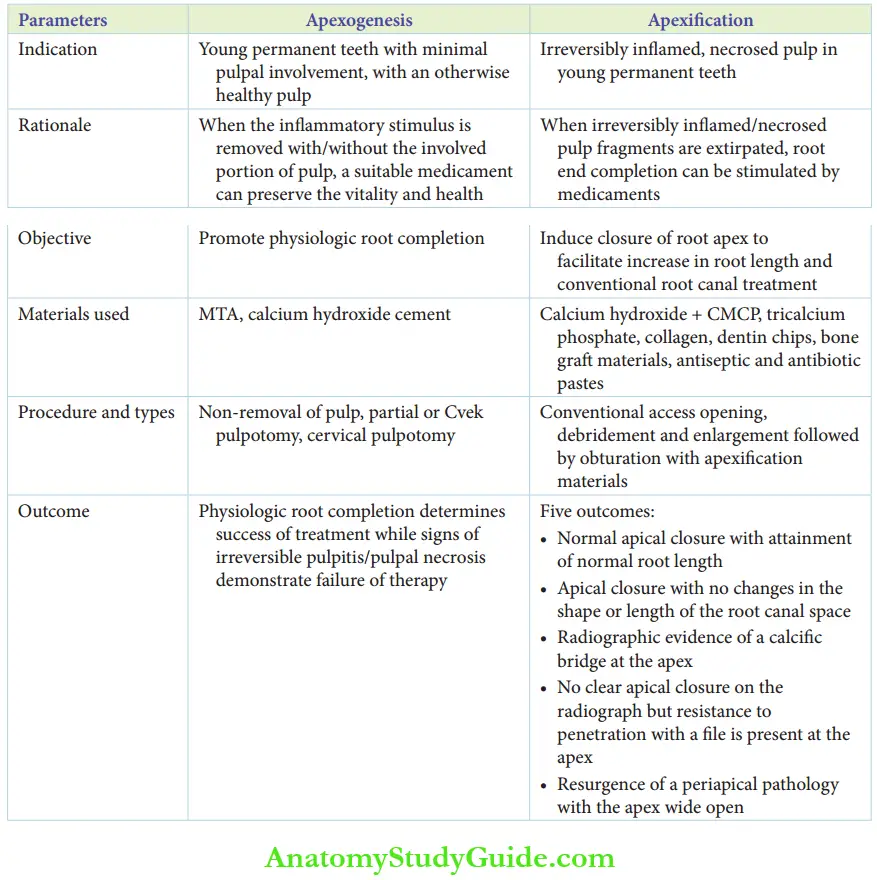
Apexogenesis
Apexogenesis is an endodontic procedure indicated in young permanent teeth with reversible pulpal inflammation. The goal is to preserve the vitality of the radicular pulp to complete root formation. The inflammatory stimulus is removed with or without the removal of the pulp tissue. Subsequently, the remaining pulp is capped with a suitable medicament to preserve its vitality. This is followed by an integral restoration to prevent micro-leakage.
The treated pulp can then complete its function of root formation. Ths, abiogenesis is a procedure that promotes physiologic root formation.
When the root formation is complete, a conventional root canal treatment with gutta-percha obturation is performed on the tooth. This is because inflammatory stimuli may be present innocuously and can flare up in the long run.
- Indications Apexogenesis is indicated on:
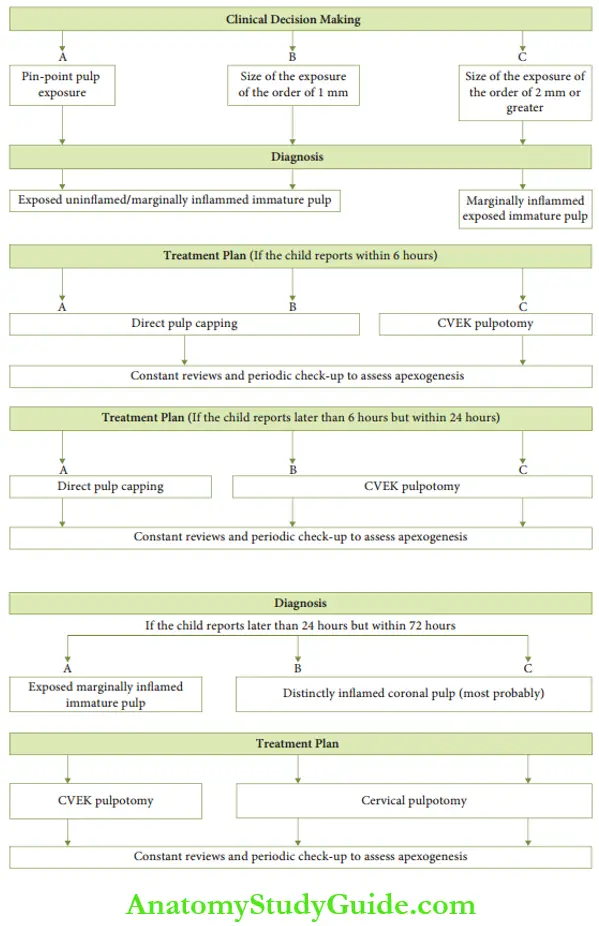
- Immature teeth within 24 hours of traumatic pulp exposure
- Immature teeth with pulp exposure on complete caries excavation, but with no symptoms of irreversible pulpitis
- Procedure Apexogenesis is carried out under local anesthesia and rubber dam isolation. The pulpal wound is irrigated and all the debris is cleared. Apexogenesis can be performed by either of the three methods, namely pulp capping, partial or Cvek pulpotomy, and cervical pulpotomy.
- Non-removal of the pulp: When the traumatic pulp exposure is extremely small or a pin-point exposure, the pulp tissue is not removed. It is left intact. The procedure is similar to a direct pulp capping procedure.
- Partial or Cvek pulpotomy: When the traumatic exposure is of size 2 mm or when the exposure fol lows caries excavation, a Cvek pulpotomy is performed. The exposure site is slightly enlarged. A few millimeters of pulp is excavated at the exposure site with a very small and sharp cloud spoon excavator. An abrasive diamond bur or a carbide no. 330 but can be used with excessive water cooling to remove the tissue. The amputated surface must demonstrate a healthy pulp with no bleeding. If bleeding persists, it implies that the inflamed pulp exists beyond the line of amputation from Cvek pulpotomy. This demands a deeper removal of the coronal pulp. Cervical pulpotomy is done in such cases. If the hemostasis is obtained, the healthy pulp is covered with a medicament, and an entrance restoration is done. This is explained in cervical pulpotomy
- Cervical pulpotomy: This is performed when one is unable to excise an inflamed pulp by Cvek pulpotomy and achieve hemostasis on the cut surface. In cervical pulpotomy, the fracture site is enlarged with a round bur for access, or a total cavity is prepared to gain better access. The pulp is amputated up to the level of the gingival crest of the alveolar bone with a sharp spoon excavator. The amputated surface must demonstrate a healthy pulp with no bleeding. The pulp is well irrigated with saline to remove debris. A moist cotton pellet is used to obtain homeostasis with gentle pressure application. The medicament of choice is calcium hydroxide cement. Recently, MTA has been increasingly and successfully employed. The medicament is placed on the pulp tissue and care is exercised so that it is not kept on a bleeding pulp or a blood clot. A thick mix of zinc oxide eugenol is placed followed by glass ionomer cement to seal the access cavity. This prevents microleakage. A full-coverage semi-permanent restoration is done after that. A provisional light-cure composite restoration is also useful.
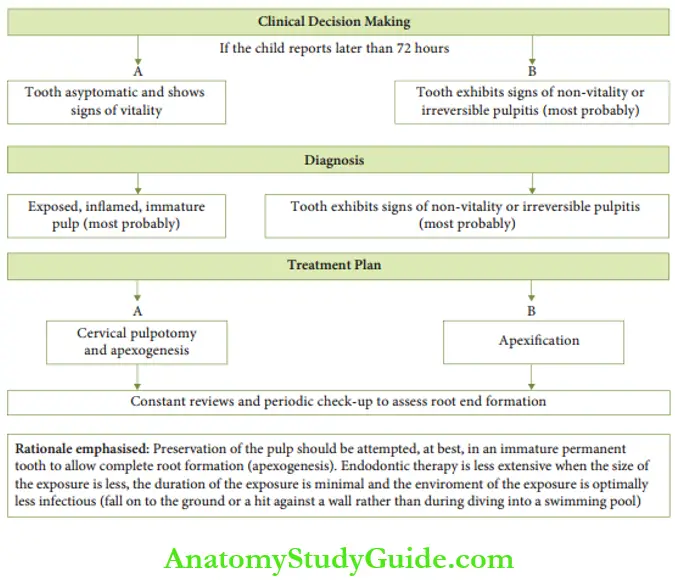
- Review The review is structured once in 3 months. A clinical and radiographic examination is required to assess the treated tooth.
- Clinical review: This is done to check for signs of irreversible pulpitis, pulp necrosis or non-vitality. The signs and symptoms may be spontaneous persistent pain, discoloration, abscess/sinus formation, or mobility. If the apex is still immature at the time of presentation of symptoms, apexification is the treatment of choice.
- Radiographic review: An IOPA radiograph is taken to assess root completion. This is noted by the narrowing of the apical foramen. When root formation is complete, conventional root canal treatment is done with gutta-percha obturation.
Apexification
Apexification is the procedure of inducing root end closure in non-vital teeth with an immature wide-open apex. The necrosed pulp does not perform its function of inducing spontaneous root end closure.
- Medicaments Calcium hydroxide cement and MTA are the materials of choice. Th other recommended materials are as follows:
- Paste of calcium hydroxide and camphorated monochlorophenol
- Antiseptic and antibiotic paste
- Tricalcium phosphate
- Collagen
- Dentin chips – hydroxyapatite crystals
- Bone graft materials
- Zinc oxide and camphorated monochlorophenol (CMCP)
- Procedure In apexification, the necrotic pulpal remnants need to be removed to eliminate focal sepsis. The procedure is carried out under local anesthesia and is best done with rubber dam isolation. An access cavity is prepared and pulpal fragments are extirpated. A thorough biomechanical cleansing of the canal is done. In teeth with sinuses, curettage of the lesion is performed with a spoon excavator. The canal is dried and the medicament is packed along its entire length. This medicament stimulates the closure of the immature, open apex. When the medicament opted is a paste of calcium hydroxide and camphorated monochlorophenol, the technique is called Frank’s technique. Post-operative radiographs are taken to check the accuracy of the root canal filling. A thick mix of zinc oxide eugenol cement followed by glass ionomer cement is placed to seal the access cavity. The tooth is reviewed for root end closure at intervals. On root end closure, a conventional root canal treatment is done with guttapercha obturation.
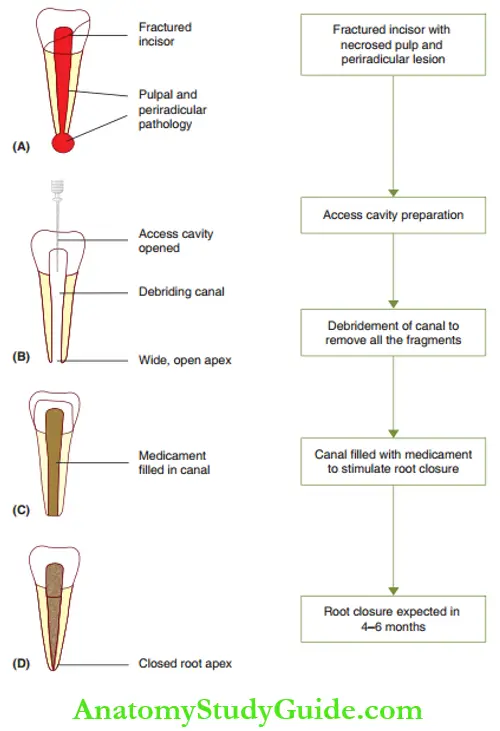
- Review Th treated tooth is reviewed 4 weeks later and once in 6 weeks thereafter. The 4-week review is a clinical review to ensure that the symptoms of irreversible pulpitis, pulpal necrosis, or dentoalveolar abscess are absent. The 6-week reviews thereafter are radiographic reviews. IOPA radiographs of the treated tooth are compared with the pre-operative IOPA radiograph to assess root end closure.
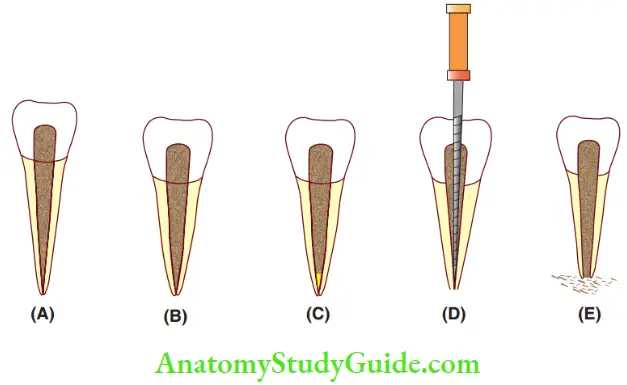
1. (A) Normal apical closure.
2. (B) Normal apical closure with no further increase in root length.
3. (C) Radiographic evidence of a calcified bridge at the apex.
4. (D) No apical closure but with an apical barrier.
5. (E) The resurgence of pathology.- Five outcomes are possible after an apexification procedure, which is as follows:
- Normal apical closure with the attainment of normal root length
- Normal apical closure, but with no further increase in root length
- Radiographic evidence of a calcified bridge at the apex
- No clear apical closure on the radiograph but resistance to penetration with a fie is present at the apex
- The resurgence of a periapical pathology with the apex wide open
- Five outcomes are possible after an apexification procedure, which is as follows:
Root end closure is best expected in 4 -6 months. Conventional root canal treatment with guttapercha obturation is carried out in case of the first four outcomes. A repeat apexification procedure or extraction is the treatment option in case of the occurrence of the fit outcome. The choice is based on the amount of bone loss and root resorption.
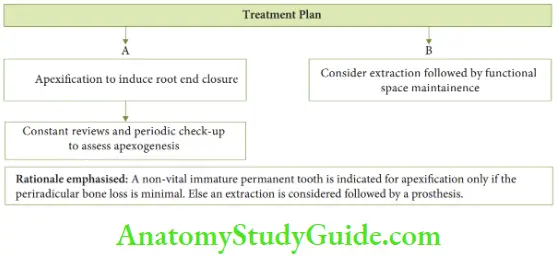
Case Description
Case 1
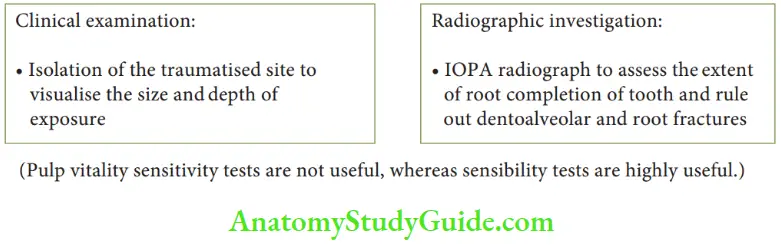
- Chief complaint: A 7½-year-old male child complains of fall and bleeding from the right upper front tooth there are.
- Clinical scenario: A 7½-year-old child underwent a fall injury and fractured his right maxillary central incisor. He presents with bleeding from within the tooth. e surrounding structures of the tooth are intact. [Baseline data – Maxillary central incisor is an immature permanent tooth in a 7-year-old child]
Case 2
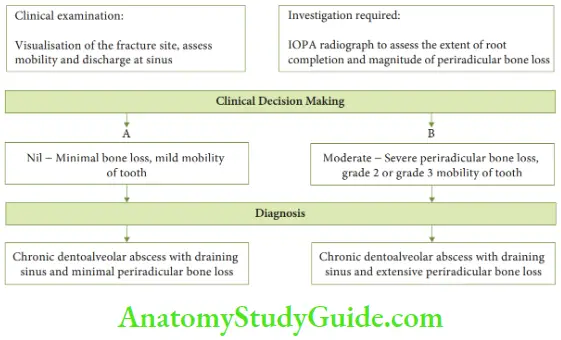
- Chief complaint: An 8-year-old boy complains of a discolored right upper front tooth and gives a history of falls before 1 year.
- Clinical scenario: An 8-year-old boy reported a complaint of discharge and mild mobility associated with a discolored right maxillary incisor fractured 1 year ago. [Baseline data – An 8-year-old presents an immature permanent central incisor.]
Summary
- Clinical significance of a young permanent tooth
- Pulp capping
- Apexogenesis versus apexification
Leave a Reply