Salient Differences Between Physical Examination Of Children And Adults
General Differences
Table of Contents
1. History is often imprecise because the child cannot express or explain his problems. The accuracy of history depends upon the intelligence, education, observational ability, and concern of the mother, father, or attendant.
2. Dietary and immunization history is of special significance among children. Children are prone to develop protein-energy malnutrition and deficiency of micronutrients. Perinatal events, growth, and developmental history should be enquired and recorded, especially in preschool children.
3. There is a general lack of cooperation by the child during the examination. Observation is most contributory or informative in children and should be accorded maximum importance.
4. The approach during clinical examination does not follow any set sequence but is unstructured. The unpleasant examination is postponed to the end. Children must be handled as children and not as patients.
5. Childhood period is characterized by rapid growth and development. A pediatrician, therefore, deals with subjects varying in weight from 1.0 to 50 kg and in different stages of maturation. Examination tools of different sizes are needed depending upon the age of the child example size of the stethoscope, ear specula, cuff of blood pressure apparatus, little finger for a rectal examination so on and so forth.
6. Developmental defects, chromosomal disorders, and inborn errors of metabolism are by and large limited to children and should be looked for.
Read and Learn More Pediatric Clinical Methods Notes
General Physical Examination
1. Anthropometry is of particular importance and of special significance in children. The availability of electronic weighing scales for infants and children and infantometer for infants and stadiometer for older children is mandatory.
2. Developmental assessment is peculiar to children.
3. Disorders of head size and shape are limited to children because of open sutures and fontanels.
4. Infants are more likely to have sacral edema and puffiness of the face instead of pedal edema.
5. Peculiar and diagnostic facies (dysmorphism) and developmental disorders are by and large limited to children.
6. Deficiency states are far more common among children because of greater caloric and nutritional needs per unit body weight, reduced dietary intake, and dependence on caretakers to meet their nutritional requirements. Some deficiency states produce different manifestations among children as compared to adults, e.g. rickets vs osteomalacia.
7. Signs of meningeal irritation may be minimal or absent during the first year of life (especially
first 3 months) and in malnourished children.
8. Lymphoid hyperplasia is marked during the preschool period, leading to adenoidal hypertrophy, and enlargement of tonsils and cervical lymph nodes.
9. Iron deficiency is common but koilonychia is rare among children.
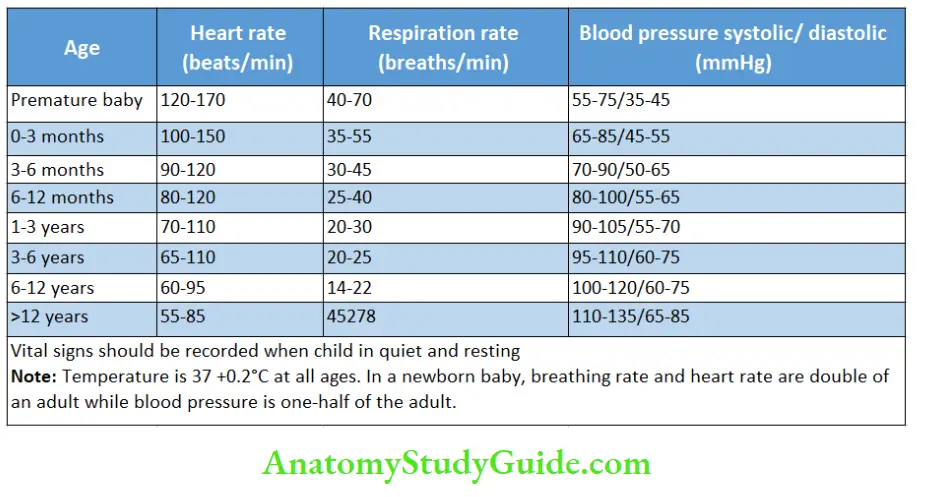
10. The norms for vital signs are different in children of different ages. Heart rate(pulse rate) and breathing rates should be recorded for one minute when a child is quiet, resting, or asleep.
Systemic Examination
Alimentary System
1. Abdomen is protuberant (pot-belly) and soft in infants. Divarication of the recti and umbilical hernia are common.
2. Palpation of the abdomen in infants is best achieved during feeding.
3. Palpable liver up to 2 cm with soft consistency is normal throughout childhood while spleen tip may be normally felt during the first 3 months of life.
4. Genital area should be routinely examined to look for congenital malformations, inguinal hernia, hydrocele, and undescended testis.
Respiratory System
1. The breathing is rapid and abdominothoracic in infants. The normal rhythm is inspiration expiration – pause. It gets reversed to expiratory grunt – inspiration – pause in respiratory distress syndrome and pneumonia. Intercostal and suprasternal recessions are common due to soft ribs
2. Chest deformities (Pigeon chest and funnel-shaped chest) and Harrison’s sulcus may occur in children with rickets and recurrent respiratory infections and obstructive airway disease.
3. Narrow air passages predispose to frequent development of stridor, wheezing, and atelectasis.
4. Percussion may be impaired over the manubrium site due to enlarged thymus. The chest is more resonant in children as compared to adults because of the thin chest wall.
5. The normal breath sounds are hollow and puerile or harsh vesicular in children. Due to the small thorax, the adventitious sounds from one side may be conducted to the opposite side.
Cardiovascular System
1. Pulse is rapid and difficult to feel among infants due to the small size of the wrist and decreased vagal tone. Sinus arrhythmia, i.e. increase in heart rate during inspiration and bradycardia on expiration, is common in children.
2. Jugular venous pressure is difficult to evaluate in infants because of the short and obese necks.
3. It is preferable to auscultate the heart of an infant first before he starts crying due to palpation and percussion.
4. Precordial bulge may occur as a sign of long-standing cardiac enlargement because of a soft rib cage.
5. Apex beat is located in the 4th intercostal space at or slightly outside the midclavicular line.
6. Splitting of the second heart sound is common. P2 is louder than A2 in infants up to 6 months of age. Heart sounds are better audible due to the thin chest.
7. Functional systolic murmurs and venous hum are common in children.
8. Right ventricular hypertrophy is seen in newborn babies while left ventricular preponderance occurs in adults.
9. Blood pressure is lower in children and proper cuff size (to cover two-thirds of the upper arm) is essential for recording it. The flush method or Doppler system may have to be used to record blood pressure in infants.
10. Most congenital cardiac defects produce their clinical manifestations during early childhood while rheumatic heart disease is unlikely below the age of 3 years.
Central Nervous System
1. Cooperation for proper CNS examination of children is exceedingly difficult. Several tricks or play attitudes may have to be adopted for thorough CNS assessment. Sensations are the most difficult to assess.
2. The likelihood of neurological symptoms, like alteration in consciousness and seizures, being due to disease outside the CNS (due to toxins and metabolic disorders) is more likely in children than adults. Febrile seizures are limited to children between 6 months and 5 years of age.
3. Several primitive or automatic reflexes (Moro reflex, palmar grasp, neck tonic reflex) are present at birth and they disappear by the age of 4 to 5 months. Their persistence is indicative of brain damage.
4. Developmental screening is a part of CNS evaluation in children. Delay in the appearance of the social smile, persistence of automatic reflexes, neck tonic posture, clenched fists, increase in muscle tone, inability to follow light/red ball, and delay in achieving motor skills are useful early markers of cerebral palsy.
5. Deep tendon jerks are normally brisk during infancy. When knee jerk is elicited on one side, crossed adductor response may be seen in normal infants. The cremasteric response is also exaggerated in infants and may be preserved even when there is other evidence of pyramidal involvement. It may be lost in a child with torsion of the testis.
6. Plantars may be normally extensors on both sides in infants up to 2 years of age. The presence of unilateral extensor plantar reflex is more significant at this age.
7. Fundus examination reveals that the optic disk is normally pale in infants. Papilledema appears only after 2 to 3 years of age when sutures have closed.
Leave a Reply