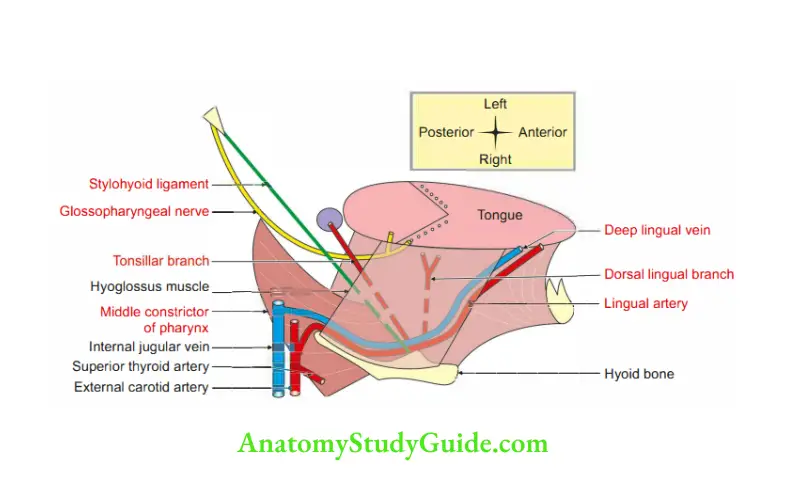
Relations of hyoglossus muscle
1. Superficial structures are grouped as
1. Nerves
Table of Contents
- Hypoglossal nerve-12th cranial nerve, and
- Lingual nerve, a branch of posterior division of mandibular division of trigeminal nerve.
Read And Learn More: Face Anatomy Notes And Important Questions
2. Muscle: Styloglossus
3. Structures related to word IIsubmandibular”
- Submandibular ganglion,
- Deep part of the submandibular gland, and
- Submandibular duct.
4. Veins accompanying it.
2. Deep
1. Nerve: Glossopharyngeal nerve-9th cranial nerve.
2. Artery: Lingual artery, a branch of external carotid artery.
3. Muscles
Muscle of tongue
- Inferior longitudinal muscle of the tongue.
- Genioglossus.
Muscle of pharynx: Middle constrictor of the pharynx.
4. Ligament: Stylohyoid.
3. Structures passing deep to posterior border of hyoglossus, from above downwards are
- Glossopharyngeal nerve.
- Stylohyoid ligament.
- Lingual artery.
Mylohyoid muscle (oral diaphragm)
Introduction: It forms the diaphragm of the floor of the mouth.
1. Proximal attachments: It arises from the mylohyoid line present in the inner surface of body of mandible.
It extends from 3rd molar tooth to mental spine.
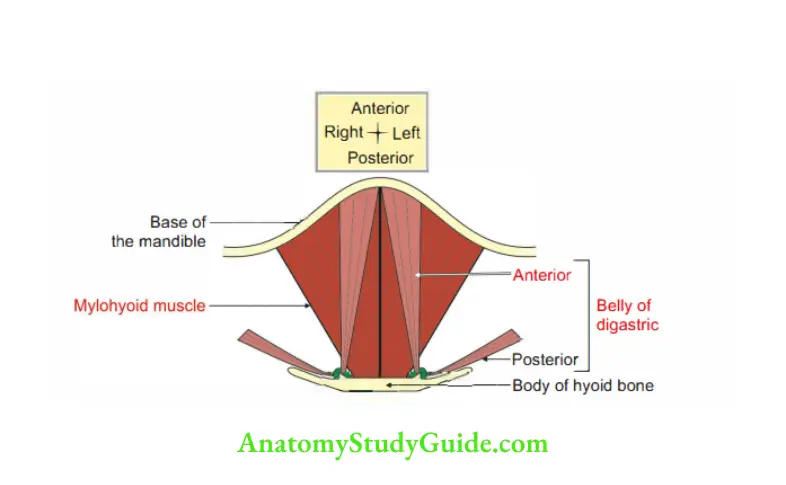
2. Distal attachments
- Anterior¾ fibres interdigitate with each othr in the midline. They extend between the symphysis menti and the hyoid bone and form mylohyoid raphe.
- It is only the posterior fibres which get inserted into the anterior surface of the body of hyoid bone.
3. Nerve supply: Nerve to mylohyoid, a branch of inferior alveolar nerve, branch of posterior division of mandibular nerve.
Note: Nerve to mylohyoid pierces sphenomandibular ligament and supplies
1. Mylohyoid.
2. Anterior belly of digastric
4. Action: It elevates tongue and hyoid bone during swallowing.
5. Relations: The submandibular gland is the main relation to mylohyoid muscle.
It has larger superficial and smaller deep part.
6. Development: It develops from mesenchyme of 1st pharyngeal arch.
Carotid nerve
1. Carotid nerve: The internal carotid nerve arises from the upper end of the superior cervical sympathetic ganglion.
It accompanies the internal carotid artery into the skull and forms the internal carotid plexus.
The fibres from the plexus are distributed to
- All branches of the internal carotid artery,
- Pterygopalatine ganglion,
- Eyeball, and
- Dilator pupillae of the iris.
2. Features
- It is composed mainly of postganglionic fibres arising from the superior cervical ganglion.
- The nerve ascends along the internal carotid artery. It divides into branches that form a plexus over it.
- This plexus has numerous connctions.
3. Connections:
1.In the carotid canal, it forms caroticotympanic nerves.
It enters the middle ear cavity and participates in the formation of tympanic plexus.
2. In the foramen lacerum, the plexus around internal carotid artery is called deep petrosal nerve.
It joins the greater petrosal nerve and forms the nerve to the pterygoid canal (nerve of Vidian canal).
- The fibres reach the pterygopalatine ganglion.
- They pass through the ganglion without relay and travel through the orbital branches. They supply the orbitalis muscle.
3. In the cavernous sinus, it communicates with the ophthalmic division of the trigeminal nerve.
These fibres pass through nasociliary nerve.
They travel through the long ciliary nerves and reach the eyeball. They supply the
- Dilator pupillae muscle, and the
- Blood vessels of the eyeball.
4. These fibres pass through ciliary ganglion without relay and then pass into the short ciliary nerves to supply the blood vessels of the eyeball.
5. It may be noted here that preganglionic sympathetic fibres for the eyeball begin in segment Tl of the spinal cord and ascend in the sympathetic trunk to the superior cervical ganglion in which the postganglionic neurons lie.
Question 1: What are the parts of submandibular gland?
Answer: 1. Superficial part of submandibular gland.
2. Deep part of submandibular gland.
Question 2: Where is the opening of submandibular duct?
Answer: It opens in the floor of the mouth.
It is on the summit of the sublingual papilla.
It is demonstrated at the side of the frenulum of the tongue.
Question 3: Why the” incision for removal of submandibular gland is placed more than below the angle of mandible?
Answer: The marginal mandibular branch of the facial nerve is situated at posteroinferior angle of jaw. To avoid the injury to the nerve, the incision is always taken 1″ below the angle of mandible.
Question 4: Describe submandibular gland under the following headings:
1. Morphology
2. Relations
3. Blood supply
4. Lymphatic drainage
5. Nerve supply
6. Applied anatomy
1. Morphology: This is a large salivary gland situated in the anterior part of digastric triangle, in the submandibular region of mandible.
It extends up to stylomandibular ligament.
Division: The gland is divided by mylohyoid muscle into
- Large superficial part, and
- Small deep part.
Ends: It has two ends:
- Anterior, and
- Posterior.
Presents three surfaces
- Inferior,
- Lateral, and
- Medial.
2. Relations: Submandibular gland has larger superficial part and smaller deep part.
1. Superficial part
Relations of inferior surface
- Skin,
- Superficial fascia,
- Platysma,
- Deep fascia,
- Common facial vein,
- Cervical branch of facial nerve,
- Submandibular lymph node.
Relations on lateral surface
- Submandibular fossa of mandible,
- Medial pterygoid muscle, and
- Facial artery.
Medial surface is extensive and divided into three parts:
1. Anterior
- Mylohyoid muscle,
- Mylohyoid vessels,
- Mylohyoid nerve, and
- Submental branch of facial artery.
2. Intermediate
- Hyoglossus,
- Lingual nerve,
- Submandibular ganglion,
- Hypoglossal nerve, and
- Intermediate tendon of digastric.
3. Posterior
- Styloglossus,
- Stylopharyngeus,
- Digastric,
- Middle constrictor of pharynx,
- Hypoglossal nerve, and
- Lingual artery.
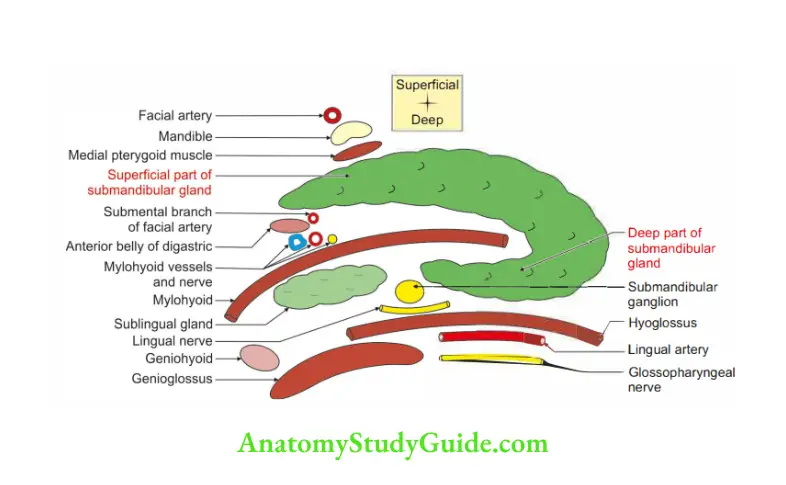
Deep part:
- Laterally: Mylohyoid.
- Medially: Hyoglossus and styloglossus.
3. Blood supply
- Arterial supply: Glandular branch of facial artery.
- Venous drainage: Common facial or lingual vein draining into internaljugular vein.
4. Lymphatic drainage: Submandibular lymph nodes.
5. Nerve supply
1. Secretomotor fibres: Arise from superior salivatory nucleus .
- Preganglionic fibres pass through facial nerve>chorda tympani> lingual nerve>submandibular ganglion.
- Post-ganglionic fibres arise from ganglion and enter submandibular gland.
- Sensory fibres reach the ganglion through lingual nerve, branch of mandibularnerve.
- Sympathetic fibres arise from superior cervical sympathetic ganglion. These fires do not relay in the submandibular ganglion.
6. Applied anatomy
- The mandibular branch of facial nerve is closely related to the angle of jaw.
The submandibular gland is excised by an incision 1″ below the angle of jaw. - The secretion of the submandibular gland is more viscous; hence, the incidence of calculi is more common in the submandibular gland.
- A stone in the submandibular duct (Wharton’s duct) can be palpated bimanually in the floor of the mouth and can even be seen, if sufficiently large.
Submandibular lymph nodes
1. Situation: They are situated in the digastric triangle beneath the deep cervical fascia.
A few are embedded in the substance of submandibular salivary gland.
2. Number: They are usually three in number.
- One in front of facial artery.
- One behind the facial artery.
- One on the anterior border of submandibular gland.
3. Relation: They are crossed by mandibular branch of facial nerve.
4. Afferent
- Centre of forehead,
- Medial angle of the eye,
- Side of nose,
- Cheek and angle of mouth,
- Whole of upper lip,
- Lateral part of lower lip,
- Anterior two-thirds of tongue,
- Upper gum through infraorbital foramen,
- Lower gum through the mental foramen, and
- Most of the air sinuses.
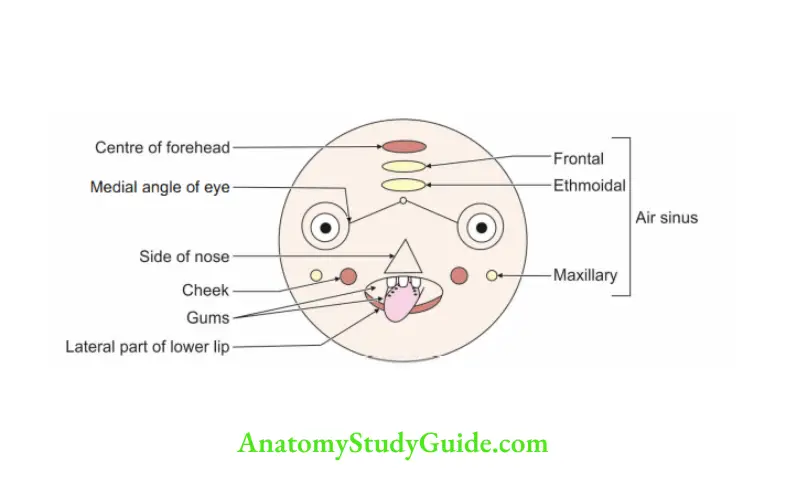
5. Efferent
- Jugulo-omohyoid
- Jugulodigastric.
6. Applied anatomy: In malignancy of mandible, the submandibular gland along with submandibular lymph nodes is removed in the block dissection called hemi mandibulectomy.
Histology of submandibular gland
The letters of the word signify the type of secretion they produce.
Parotid- Pure serous.
sub- mandibular: esrous more (predominantly serous)
sub- lingual: serous less (predominantly mucous)
- It is very simple to remember the types of salivary gland.
There are mainly three salivary glands, namely parotid, submandibular and sublingual. - Parotid is pure serous, submandibular and sublingual are mixed.
- Submandibular is predominant serous.
- Sublingual is predominantly mucous.
- Use the letter “P” for pure, .
- Letter “M” for more, and the
- Letter “L” for less, things are easy to remember.
- parotid gland: The word “farotid” begins with the letter “£”, hence remember parotid is pure serous.
- Sub-mandibular gland has letters “S” and the letter “M”, hence serous more, i.e., predominant serous.
- Sub-lingual gland has the letters “S” and the letter “1” hence serous less, i.e.,predominant mucous.
Featues
1. Submandibular gland is mixed, predominantly serous salivary gland.
2. No lymphoid tissue.
3. Typical connective tissue—-ce, septa and stroma are present.
4. The parenchyma is divided by septa into lobules.
5. Most of the mucous secretory units are capped by serous demilunes (1/2 moon)
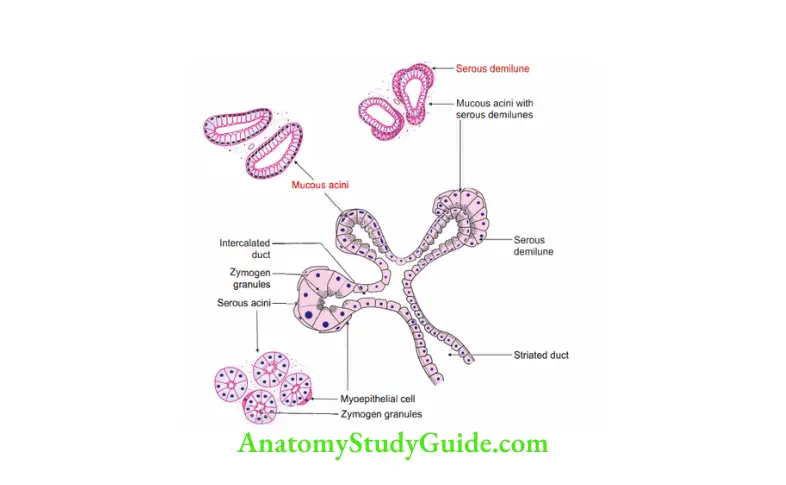
6. Serous secretory units have a round nucleus which is located near the centre of the cell.
This is in contrast with the mucous cells which have a flattened nucleus. It is pressed against the base of the cell.
7. Presence of myoepithelial cells in relation to acini.
8. Interlobular excretory ducts are located in the interlobar connective tissue septa.
The septa divide the gland into lobules and lobes.
9. Intralobular ducts join to form the interlobular ducts and interlobar ducts.
The terminal portion of these large ducts conveys saliva from salivary gland to the oral cavity.
It constitutes the main ducts of each salivary gland.
As these interlobular and interlobar excretory ducts get larger and larger, the lining epithelium goes on changing.
The change is from stratified low cuboidal to stratified columnr cells.
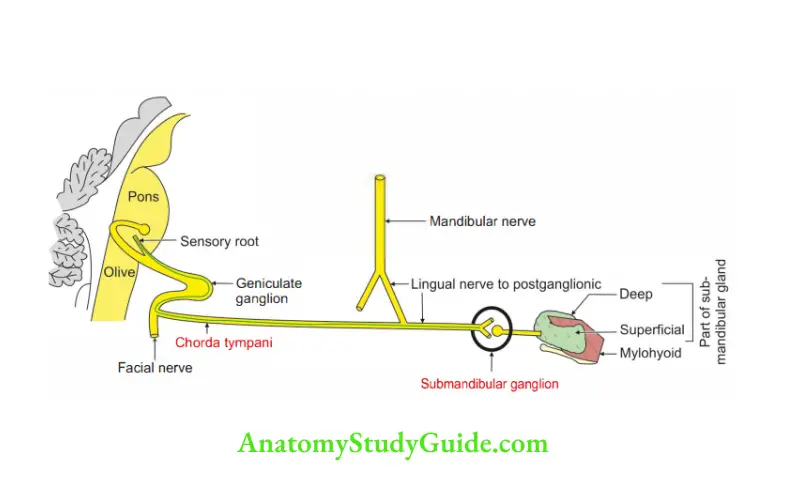
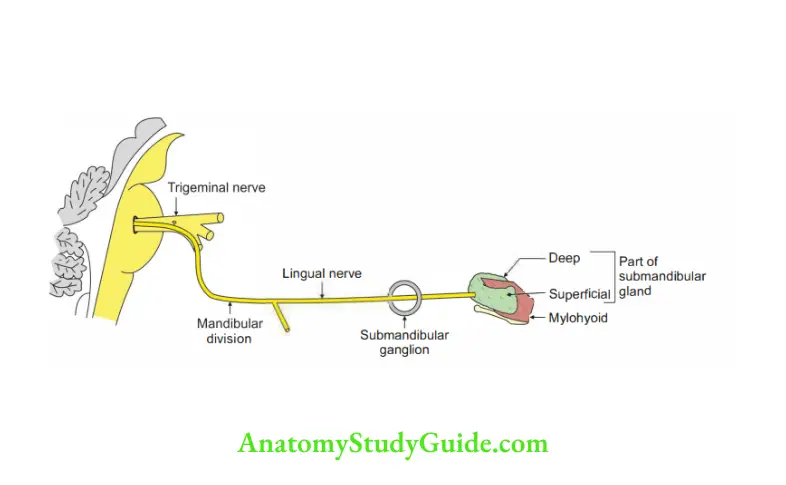
Submandibular ganglion
Introduction: It is a collection of cell bodies present in the course of parasympathetic nerve situated on the hyoglossus muscle, supplying the submandibular and sublingual glands.
- It is topographically connected to lingual nerve, branch of mandibular nerve.
- It is functionally connected to facial nerve.
1. Gross anatomy
- Shape: Fusiform ,.
- Situation: On hyoglossus muscle.
- Relations
Superior: Lingual nerve.
Inferiorly: Deep part of submandibular gland. - Connections
Parasympathetic.
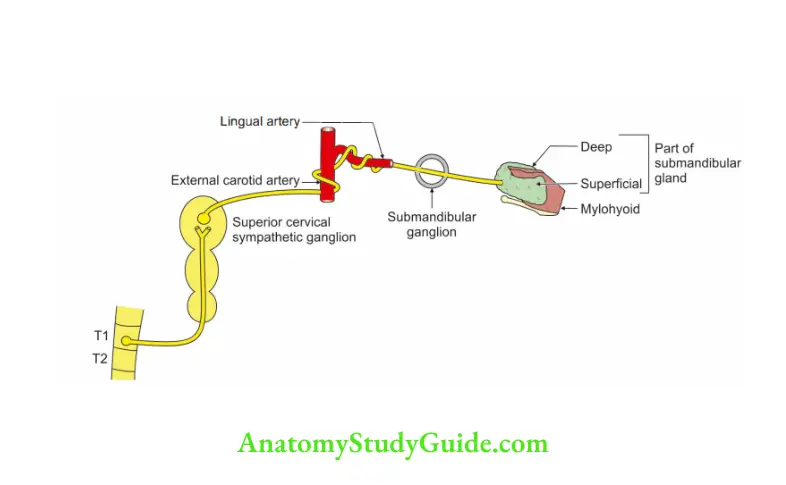
- Preganglionic fibres: Superior salivatory nucleus>facial nerve>chorda tympani joins with lingual nerve>submandibular ganglion>relay.
- Postganglionic fires: Unnamedbranches-to submandibularor sublingual gland.
2. Sympathetic fibres :
- Preganglionic fibres arise from spinal nerves>superior cervical sympathetic ganglion>fibres relay in the ganglion.
- Postganglionic fibres form the plexus around external carotid artery>(lingual artery) the fibres do no relay.
3. Sensory: Lingual nerve, a branch of mandibular division (V3) of trigeminal nerve.
2. Branches: 5 to 6 branches enter the submandibular, sublingual and anterior lingual glands.
Hyoglossus muscle
1. Origin: It arises from
- The length of greater horn of hyoid bone.
- Lateral part of the body of hyoid bone.
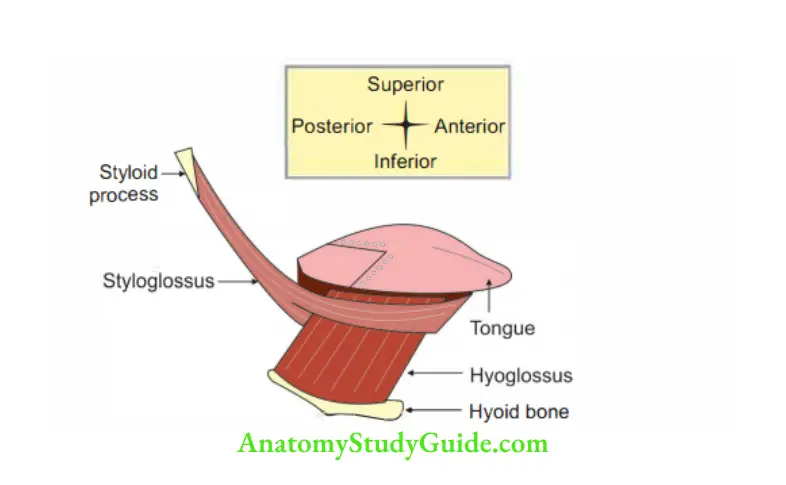
2. Insertion: Upper border interdigitates at right angles with the styloglossus and is attached to the side of tongue.
3. Nerve supply: Hypoglossal nerve-12th cranial nerve.
4. Action: It depresses the tongue.
5. Relations
1. Superficial from above downwards l”Yes” between 2 “No”
- Lingual branch of mandibular nerve
- Smandibular duct
- Hypoglossal nerve.
2. Deep relations from above downwards lying on middle constrictor of phary x are
- Glossopharyngeal nerve,
- Stylohyoid ligament, and
- Lingual artery
Leave a Reply