Replantation
Grossman, in 1982, defined intentional replantation as “the act of deliberately removing a tooth and following examination, diagnosis, endodontic manipulation, and repair—replantationreturning the tooth to its original socket.”
Table of Contents
Replantation Classifiation
Replantation can be of two types:
- Intentional replantation
- Unintentional replantation
Read And Learn More: Endodontics Notes
Replantation Indications
- Nonsurgical endodontic treatment is not possible due to limited mouth opening
- Calcifications, posts, or separated instruments present in canals make nonsurgical endodontics therapy difficult
- Persistent infection even after root canal treatment
- Inaccessibility for surgical approach due to anatomic factors
- Perforations in inaccessible areas where for surgery excessive bone loss in required
- Accidental avulsion, that is, unintentional replantation
- For a thorough examination of root defects like cracks or perforations.
Replantation Contraindications
- Curved and flared canals
- Nonrestorable tooth
- Moderate-to-severe periodontal disease
- Missing interseptal bone
- Presence of vertical root fractures.
Precautions to be taken during the replantation procedure:
- Root surface (with PDL cells) should be kept moist with Hanks balanced salt solution or saline during the time tooth is out of the socket
- Out-of-socket, time should be the shortest possible
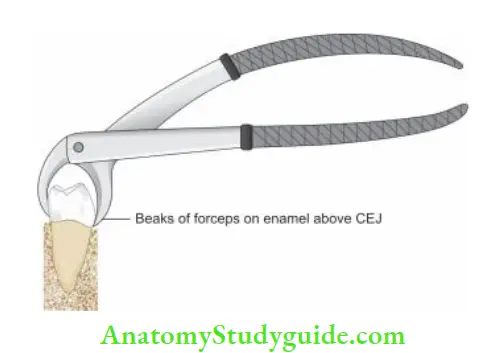
- One should take care not to damage PDL cells and cementum. Avoid touching forceps’ beaks on cementum
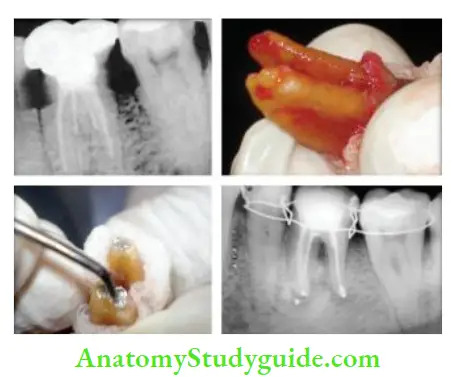
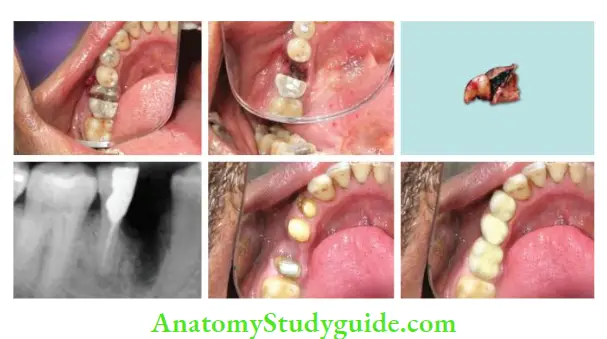
Replantation Technique
- Extract the tooth with minimal trauma to the tooth and socket
- Incise periodontal fiers using No. 15 scalpel blade
- Gently elevate the tooth using forceps in a rocking motion until grade I mobility is achieved. Forceps should be placed away from the cementum so as to avoid damage to the periodontal ligament
- Keep the root surface moist by wrapping it with gauze soaked in a physiologic solution such as Hanks balanced salt solution
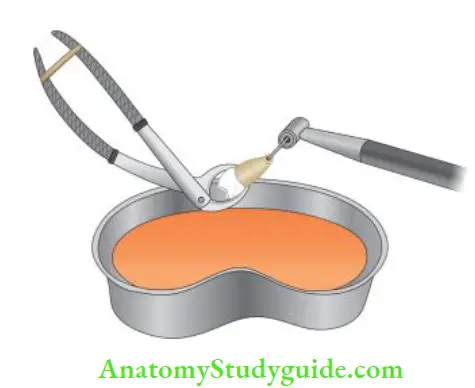
- Thoroughly examine the roots for defects or fractures and repair the defects if indicated. Any repair or procedure should be done quickly in the bath of normal saline or HBSS solution so as to prevent desiccation
- Irrigate the extraction socket using normal saline
- Gently place the tooth back in the socket and place a rolled gauze piece on the occlusal surface. Ask the patient to bite on it for at least 5–10 min. This will help in seating the tooth into the socket
- Stabilize the tooth using periopak, sutures, or splints.
- Recall the patient after 7–14 days so as to remove the stabilization and to evaluate the mobility
- Follow-up should be done after 2, 6, 9, and 12 months of surgery.
Replantation Prognosis
It depends on preventing trauma to the PDL and cementum during extraction and minimizing extraoral time.
Causes of Failure of Reimplantation
- Extended extraoral time resulting in damage to periodontal cells
- Contamination during the procedure—resulting in infection and resorption
- Undetected fracture of the tooth
- Mishandling of tooth during reimplantation procedure.
Transplantation
It is the procedure of replacement of a tooth in a socket other than the one from which it had been extracted from.
Hemisection Or Root Resection Or Root Amputation
Hemisection is defined as the removal of an unrestorable root which may be affected by periodontal, structural (cracks), and caries. Hemisection is independent of bicuspidization.
Hemisection includes the splitting of the tooth, extraction of one half, followed by a bridge whereas bicuspidization involves retaining of both the split sections of the tooth and then restoring them with crowns.
Transplantation Indications
- Extensive bone loss in relation to the root where periodontal therapy cannot correct it
- The severely curved canal which cannot be treated
- Extensive calcifications in root
- Fracture of one root, which does not involve another root
- Resorption, caries, or perforation involving one root.
Contraindications for Root Resections
- Fused roots
- Root in close proximity to each other
- Uncooperative patient
- Lack of optimal bone support for remaining root/roots
- Endodontically incompatible remaining root/roots.
Transplantation Technique
Before root resection, carry out the endodontic treatment in roots to be retained. After this, carry out root resection. There are basically two approaches for root resections:
- Vertical: Here complete root is resected along with its associated portion of the crown. Ths procedure is also called hemisection or trisection. It is done from mesial to distal in maxillary molars and buccal to lingual in mandibular molars
- Horizontal/oblique: In this, the root is resected at the point where it joins to the crown. It is also called as a root resection.
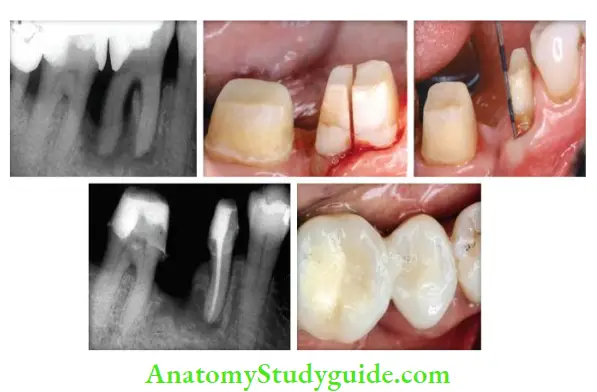
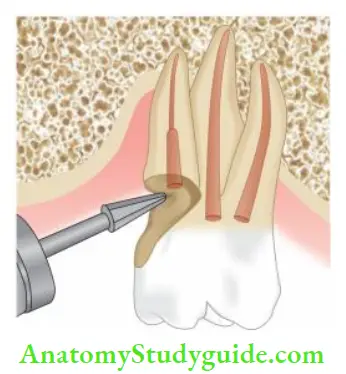
Presurgical Crown Contouring
This method involves trimming the portion of a crown over the root to be amputated so as to gain access.
Before carrying out this technique, roots should be obturated with gutta-percha. The tapered fissure bur is moved so as to trim the crown portion present to the level of the cementoenamel junction.
Bicuspidization Or Bisection
- It is defined as the surgical separation of a multirooted tooth into two halves and restoring each root with a separate crown.
- It is exclusively carried out in mandibular molars where mesial and distal roots are separated with their respective crown portions.
- Their separation eliminates the existence of furcation making the area easy to clean.
Bicuspidization Or Bisection Indications
- When periodontal disease involves the furcation area. Periodontal treatment does not improve the condition of the tooth
- Furcation is transferred to make interproximal space which makes the area more manageable by the patient.
Bicuspidization Or Bisection Contraindications
- Fused roots
- Lack of osseous support for separate segments
- Uncooperative patient.
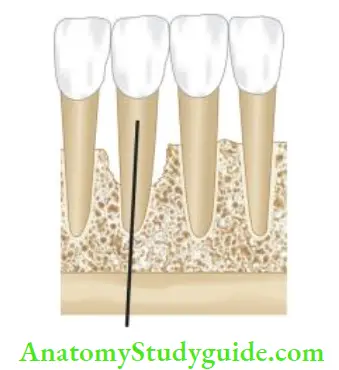
Endodontic Implants
Endodontic implants are used for providing stabilization of teeth in which alveolar support is lost due to endodontic and periodontal disease.
It enhances root anchorage by extension of artificial material beyond the alveolar socket but within range of the alveolar bone.
Case Selection for Endodontic Implants
- Teeth with straight canals
- Presence of sufficient alveolar height
- Absence of systemic disease
- Absence of any anatomic complications
- Absence of any calcifications in canals
Endodontic Implants Indications
- Horizontal root fracture
- Unaffordable root crown ratio
- Periodontally involved teeth
- Endodontically involved teeth with short roots.
Endodontic Implants Contraindications
- Presence of calcifications in roots
- Proximity of anatomic structures
- Patient suffering from systemic disease
- Presence of curved canals
Endodontic Implants Material Used for Implants
- Titanium
- Chrome cobalt alloys.
Endodontic Implants Technique
- Give local anesthesia and isolate the tooth
- Extirpate the pulp and take a working length radiograph
- Add 2–3 mm to the estimated working length so that instrument goes periodically with a minimal preparation of ISO size 60
- Start intraosseous preparation using 40 mm long reamers
- Ream the bone about 10 mm beyond the apex with sequentially increased sizes so as to achieve round apical preparation
- Complete the preparation till at least ISO No. 70, or until apex is reamed round
- Dry the canal and check the fitting of the implant. If tug back is there at working length, cut 1 mm of the apical end of the implant so as to avoid its butting against bone
- Irrigate and dry the canal, and take care not to disturb the apical clot
- Fit the canal and cut it at the point below the gingival level using a carborundum disk. One should take care that cement is applied only to the part of the implant within confines of the canal
- Seal the implant using gutta-percha
- Do coronal restoration using crown, or composite restoration.
Reasons for Failure of Endodontic Implants
- Extrusion of cementing media
- Inadequate seal at the junction of the implant and the apex
- The wrong technique of placement.
Postsurgical Care
Postsurgical Care includes providing genuine expression of concern and reassurance to the patient, good patient communication regarding the expected and normal postsurgical sequelae as well as detailed home care instructions.
Postsurgical Care Instructions
- No difficult activity or work for the rest of the day
- No alcohol or any tobacco for the next 3 days
- Good nutritious diet. Drink a lot of liquids for the first few days after surgery
- Do not lift up your lip or pull back your cheek to look at where the surgery was done. It may pull the stitches loose and cause bleeding
- A little bleeding from the surgical site is normal and it can last for a few hours. Little swelling or bruising of the face is normal and may last for a few days
- Intermittent application of ice bags on the face where surgery was done for 6–8 hours
- Take prescribed medicines regularly
- Remove the suture and make a follow-up appointment.
Suturing
A suture is a strand of material used to close the wound.
The purpose of suturing is to approximate incised tissues and also stabilize the flapped mucoperiosteum until reattachment occurs.
Classifiation of sutures
- According to absorbency
- Absorbable
- Nonabsorbable
- According to physical property
- Monofilament
- Multifilament
- Twisted or braided
Principles of Suturing
- The needle should enter the mucosal skin perpendicular to the surface of the tissue
- The needle should always pass from free tissue to fixed tissue
- The needle should always be inserted at an equal depth and distance from the incision line on both sides
- Tissue should not be closed under tension
- Sutures should be spaced evenly
- The suture should not be too tight. If sutures are too tight, there will be local ischemia underneath the suture tracks
- Suture knot should never lie on the incision line
- After tying, the knot should be left to one side.
Postsurgical Complications
Postoperative Swelling
Postoperative swelling usually reaches a maximum after 24 or 48 hours and resolves within a week.
Proper compression of surgical flp both before and after suturing reduces postoperative swelling.
Postsurgical Complications Management
- Inform the patient earlier as it reduces the anxiety
- Application of ice packs is recommended for the next 6–8 hours
- Warm saline rinses two to three times a day is recommended after 24 hours.
Postoperative Bleeding
Slight oozing of blood after surgery is normal, but significant bleeding is uncommon and may require attention.
Postoperative Bleeding Management
- The first and foremost step in managing bleeding is to apply firm pressure (with a moistened cotton gauze or a tea bag or ice pieces placed in a cotton gauge ) over the area for 10–20 min
- If bleeding still continues, then remove the sutures and search for blood vessels causing bleeding. Cauterize the blood vessel using the thermal or electrical method
- Place local hemostatics if required
- If bleeding is still unmanageable, hospitalize the patient.
Extraoral Ecchymosis (Extraoral Discoloration)
Discoloration/ecchymosis usually results when blood has leaked into the surrounding tissues.
This condition is self limiting in nature and lasts up to 2 weeks and does not affect the prognosis.
Extraoral Ecchymosis (Extraoral Discoloration) Management
Application of moist heat for 2 weeks is helpful as heat promotes fluid exchange and speeds up the resorption of discoloring agents from tissues.
Postoperative Pain
Postoperative pain is usually maximum on the day of surgery and it decreases thereafter.
Postoperative Pain Management
- Prescribe NSAIDs
- If pain is severe, opioid analgesics may be combined with NSAIDs
- Give long-acting anesthetics like bupivacaine in severe cases.
Postoperative Infection
Postoperative infection usually occurs due to inadequate aseptic technique and improper soft tissue handling, approximation, and stabilization.
Symptoms appear 36–48 hours after surgery. Suppuration, elevated temperature, and lymphadenopathy are seen in some cases.
Postoperative Infection Management
Prescribe systemic antibiotics. The antibiotic of choice in these cases is penicillin. If a person is allergic to penicillin, then clindamycin should be given (initial dose—600 mg, maintenance 150–300 mg).
Postoperative Infection Miscellaneous
- Maxillary sinusitis
- Paresthesia.
Surgical Endodontics Conclusion
The success of surgical endodontics varies between 30% and 80%. The preservation of natural teeth should be our ultimate goal because natural teeth are always far better than any man-made replacement.
Endodontic surgery is considered as last resort to save a tooth with endodontic failure.
With the advent of magnification, microinstruments, ultrasonic tips, and biologically acceptable root end filing materials, the success rate of surgical endodontics has shown to increase up to 92% along with the favorable patient response.
Leave a Reply