The Skin And Its Appendages
Skin is the largest body organ providing protective covering to the underlying structures. It is thin and more delicate in children.
Table of Contents
Over 10 percent of children reporting to the primary care physician have a dermatologic disorder.
Skin manifestations may occur due to underlying primary skin disorder or they may represent manifestations of a systemic disorder.
The number of viral exanthems is limited to children. A detailed examination of the skin and its appendages is required when primary manifestations of a disease process are limited to the skin.
Read and Learn More Pediatric Clinical Methods Notes
Skin History
Apart from demographic details, inquiry should be made regarding the duration of skin lesions, involvement of the initial site, and their subsequent progression, evolution, and distribution.
The specific areas of the skin surface involved, whether predominantly over the extensor surfaces or flexor creases should be noted.
Are skin lesions localized or generalized, symmetrical or asymmetrical in distribution? The presence of itching, irritation, and smarting sensation should be asked.
Infants manifest itching by irritability and restlessness. The presence of associated constitutional symptoms like fever, joint pains, abdominal pain, an inborn error of metabolism, or any other systemic manifestations should be looked for.
Skin manifestations may occur due to a deficiency of essential nutrients and trace elements like vitamins, zinc, and essential fatty acids.
The history of drug intake and the possibility of an adverse drug reaction should always be kept in mind.
Administration of vaccines, sera, blood, and blood components should be asked to exclude side effects of vaccines, serum sickness, and host-versus-graft reaction.
A detailed probing is required to elicit a history of contact with the offending cosmetic agents, poison ivy or toxic plant, insects (mosquitoes, ants, honey bees, centipedes, scorpions, etc.), and infested animals (fleas, visceral larva migrans, and cat scratch disease).
History of similar manifestations among household contacts is suggestive of an infective disorder like viral infection, pyoderma, and scabies.
Family history of eczema, atopic dermatitis, autoimmune disorder, vitiligo, and psoriasis should be enquired. Exclude systemic manifestations by a detailed review of body systems.
A detailed history of topical and systemic therapy taken should be recorded.
Skin Physical Examination
Examination of skin must be conducted in a well-lighted room preferably with optimal sunlight. Magnifying glass with a built-in light should be used to study the morphology of skin lesions.
A transparent spatula or glass slide is useful to view an erythematous patch after applying pressure to assess whether it blanches or not (Diascopy).
It is desirable to completely undress the young child while older children can have a loose-fitting gown.
The presence of constitutional manifestations like fever, toxemia, anorexia, and systemic symptoms demand a detailed physical examination.
Vital signs should be checked in children with a generalized skin disorders. All areas of skin including palms, soles, creases, scalp, perioral and anogenital skin should be scrutinized.
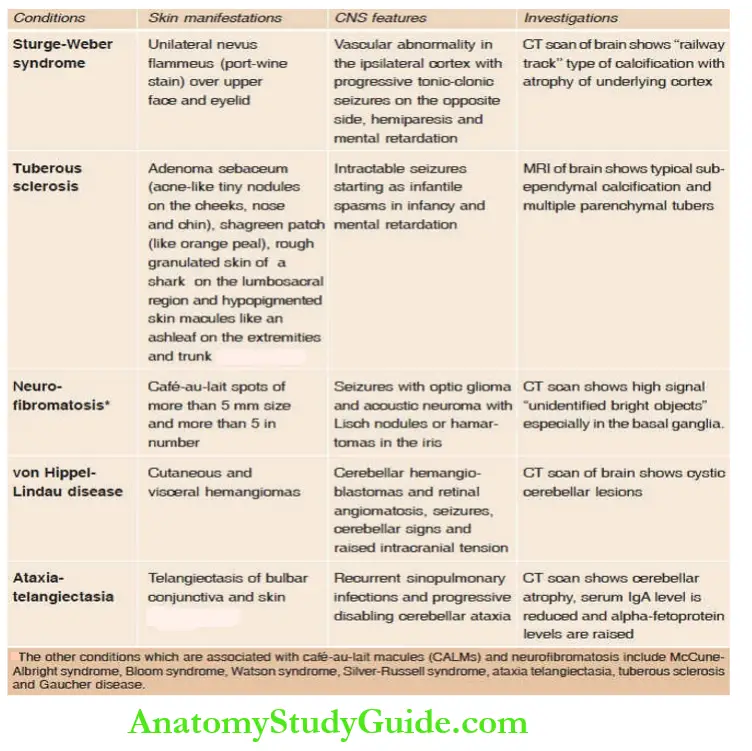
Because of the ectodermal origin of both skin and CNS, many genetic or developmental defects of the skin are associated with CNS malformations or hamartomas.
Spider nevi, palmar erythema, gynecomastia, and xanthomas may be seen in patients with chronic liver disease with hepatocellular failure.
Mucous membranes, hair, and nails are often involved in various skin disorders and should be examined in detail.
The most important aspect of the physical examination of the skin is the morphology of individual skin lesions, hi addition to a thorough inspection of the skin, palpation of skin lesions may allow the examiner to appreciate subtle depression or elevation of skin lesions.
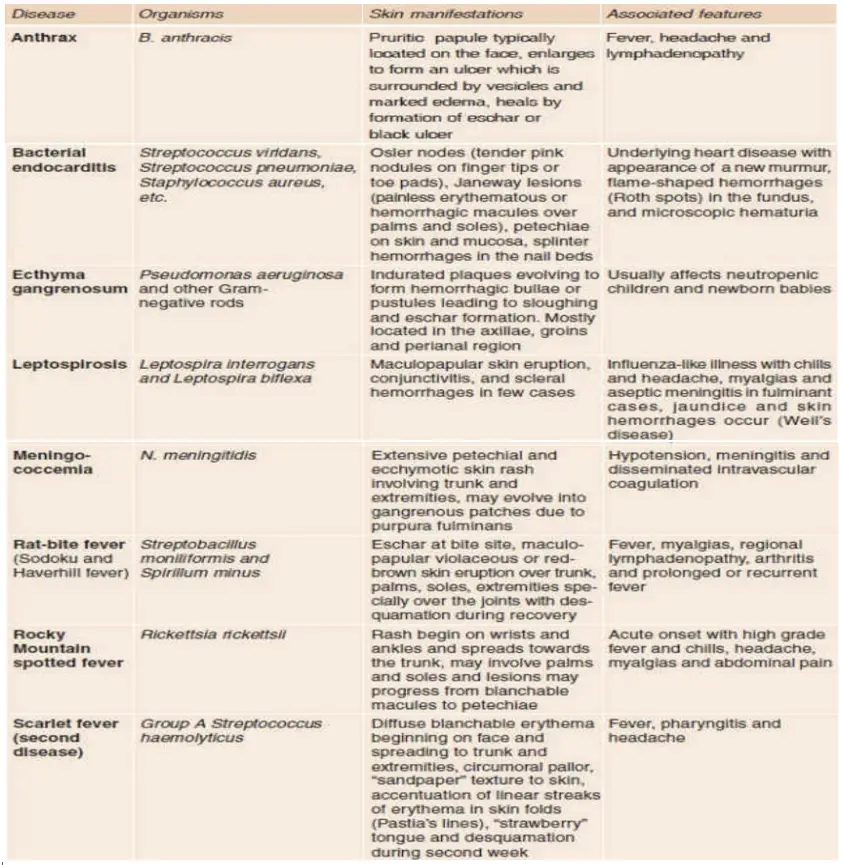
A number of viral exanthems and acute bacterial infections can be diagnosed clinically by characteristic distribution and evolution of skin rash.
The following morphologic features of skin lesions should be carefully looked for and recorded on a human diagram for their extent and distribution.
Characteristics of skin rash in common viral exanthems
1. Measles
Skin rash appears after 3–4 days of prodromal features of fever, coryza, and conjunctival congestion. The fever shoots up on the day of the onset of the rash.
Maculopapular or morbilliform confluent rash starts behind the ears and spreads to the forehead, face, neck, trunk, and extremities.
Koplik spots (grayish-white dots-like grains of sand or sago with reddish areola usually located over buccal mucosa opposite lower molars) appear 24 hours before or 24–48 hours after the onset of rash and are characteristic early markers of measles.
The rash starts to fade from the face on the third day and continues to disappear in the order of its appearance. When eruption fades, brownish copper discoloration of the skin with powdery desquamation is seen for several days.
2. Rubella (German measles)
The rash appears after 1–2 days of mild prodrome of fever, cough, and coryza. The exanthem begins on the face and extends over the body within a few hours as fine, light-pink discrete macules or scarlatiniform rash.
Suboccipital and posterior auricular lymph nodes may be slightly enlarged and tender. The rash begins to fade after 2 to 4 days leaving behind fine desquamation.
It is difficult to differentiate rubella from mild measles modified by prior immunity or immunization.
3. Chickenpox
There is no prodrome except mild symptoms of upper respiratory catarrh for one to two days.
The rash appears in crops over the trunk with a simultaneous appearance of macules, papules, and vesicles (like dew drops or teardrops) which progress to develop pustules and crusts.
Lesions spread to peripheral areas involving extremities and the face.
Pruritus is common. The crops of new lesions continue to appear over 4 to 5 days and exanthem lasts up to 8 to 14 days. Most lesions heal without scarring unless there is superadded bacterial infection.
When all the lesions are crusted, the patient is no longer contagious.
4. Erythema infectious (fifth disease)
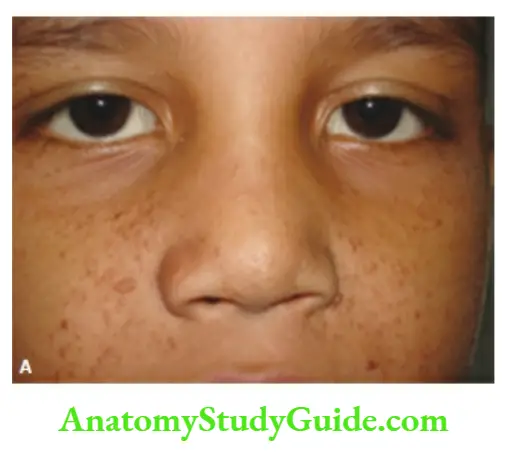
It is caused by parvovirus B19 and manifests as a bright red confluent rash over the cheeks, malar prominence, and nose giving an appearance of a ‘slapped-faceâ€. Circumoral pallor may be present.
Erythematous macules may spread over the lateral and extensor aspects of extremities, trunk, and buttocks. During recovery, there is a characteristic lace-like or reticular pattern due to the central clearing of erythematous macules.
5. Roseola infantum (exanthem subsite or sixth disease)
The onset is sudden with high-grade fever at times with convulsions. Coryza is mild or absent. The fever falls by crisis after 3–4 days followed by maculopapular skin eruption starting on the trunk and involving arms and neck.
The rash is absent or minimal on the face or legs. The skin rash fades within 24 hours without any desquamation.
6. Dengue fever
Sudden onset of high-grade continuous or saddleback or biphasic fever which comes down by lysis and profuse sweating. Fever is usually associated with headache, backache, pain in the eyes, and vomiting.
The transient maculopapular rash appears around the 3rd-4th day of fever, usually starting from the trunk and spreading to arms and legs.
There may be palmar and plantar erythema with desquamation of the skin of palms and soles during recovery.
Puffiness and swelling of the dorsum of hands and feet may occur during the stage of marked capillary permeability with the exudation of fluid into an interstitial compartment and serosal cavities.
7. Herpes simplex
There is a variable fever for 2–7 days. Papulovesicular skin lesions start from the mucocutaneous junction and spread to lips, gingivae, palate, buccal mucosa, and tongue.
The skin lesions may be widespread in children with eczema (eczema herpeticum). Skin lesions may be associated with paronychia (herpetic whitlow) and keratitis.
8. Herpes zoster (shingles)
Grouped papulovesicular skin lesions are seen with background erythema over contiguous skin dermatome in the distribution of the peripheral or cranial nerve.
The skin lesions do not cross the midline and last for 10–14 days. In adolescents, skin lesions may be associated with an intense burning sensation or excruciating pain.
The skin lesions may be widely disseminated in immunocompromised children. Varicella vaccine also provides protection against herpes zoster.
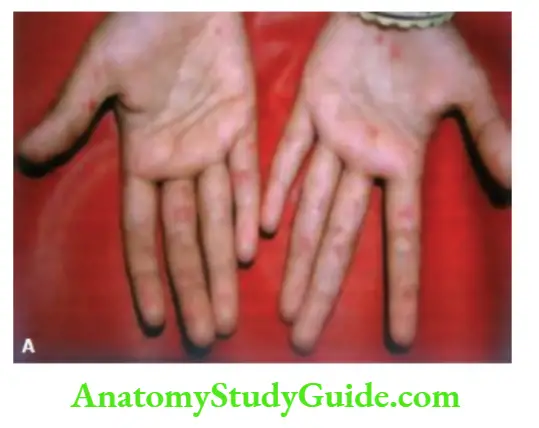
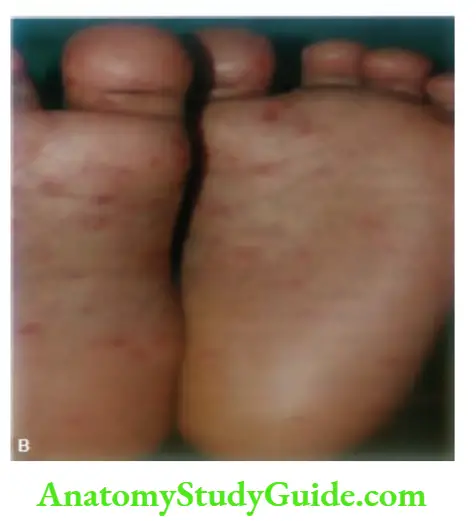
9. Hand-foot-and-mouth disease
Is usually caused by Coxsackie A16 and enterovirus 71. After an incubation period of 4 to 6 days, there is a sore throat with oral ulcerations due to vesicles over the buccal mucosa and tongue.
The fever is mild and precedes skin rash. Painful papulovesicular skin lesions appear over the palmoplantar surfaces of hands and feet, with erythematous papular skin lesions over the buttocks and thighs.
10. Infectious mononucleosis
There is a bright red morbilliform or scarlatiniform skin rash which is often precipitated by the intake of ampicillin.
The course is prolonged and there is associated generalized lymphadenopathy, herpangina (sore throat), mild jaundice, splenomegaly, and extreme fatigue.
11. Enteroviruses
Coxsackie viruses A9 and B5 and echoviruses 4, 9, and 16 may produce maculopapular, morbilliform, urticarial, or petechial skin rash. There are no characteristic or diagnostic clinical features.
12. Adenoviruses
The nonspecific maculopapular eruption is often associated with adenovirus infection
Primary Skin Lesions
Primary skin lesions provide the most vital clues for making a correct diagnosis. They are the most representative lesions of the tire disease process without any alteration by the patient by scratching, rubbing, secondary infection, or therapy.
Macules They are flat, nonpalpable areas of the color change of skin. Macules may be erythematous, hypopigmented, or hyper-pigmented.
They may be of any shape with well-defined regular or irregular borders. Examples include moles, lentigines, freckles, cafe-au-lait spots, vitiligo, Mongolian blue spot, and port wine stain.
Mole A pigmentary nevus is called a mole. Freckles They are small, less than 0.5 cm, discrete brown macules that appear on the sun-exposed areas of skin.
The condition is inherited as an autosomal dominant trait in light-skinned red-haired people. They are commonly seen on the face, back, and upper shoulders, sparing the mucous membranes.
Lentigines They are small, less than 0.5 cm, single or multiple brown to black, variegated, or uniformly colored macules over the skin or mucosae.
They are darker in color than freckles and are not affected by sunlight. They may be associated with LEOPARD syndrome, FACES syndrome, Sotos syndrome, LAMB syndrome, NAME syndrome, and Peutz-Jeghers syndrome.
Papules They are circumscribed raised skin lesions of less than 1.0 cm in diameter. They may be dome-shaped, flat-topped, conical, umbilicated, or verrucous.
Examples include molluscum contagiosum, warts, and miliaria rubra (prickly heat). Papilloma is a pedunculated lesion projecting from the skin.
Nodules are elevated skin lesions larger than 1.0 cm in diameter. They may be located in the epidermis, dermis, or subcutaneous tissue.
Examples include epidermoid cysts, fibromas, and neurofibromas. Tumors are large nodules, generally >2 cm in diameter. They may be benign or malignant and primary or metastatic.
Plaques They are well-circumscribed, broad-based diploid lesions of altered skin texture often formed by the coalescence of a number of papules.
The diameter or size of the lesions is greater than its height or elevation. A plaque may be flat, elevated, or depressed. A typical example is psoriasis.
Target lesion Annular patch or plaque with central vesicle or pigmentation and a halo of erythema (erythema multiforme).
Wheels They are transient, raised, edematous skin lesions with irregular edges. The lesions are erythematous with a central pallor. Intense itching is usually present.
They can be seen by dermatographism (Darier’s sign and tache cerebral), arid show characteristics of urticaria, and insect bites.
Vesicles The elevated, fluid-containing skin lesions or blisters of <1.0 cm diameter are called vesicles. Examples include chickenpox, herpes simplex or zoster, and contact dermatitis.
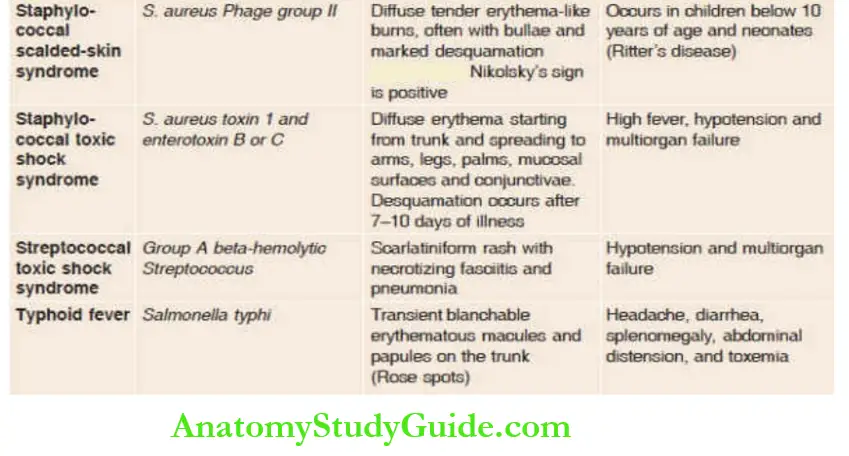
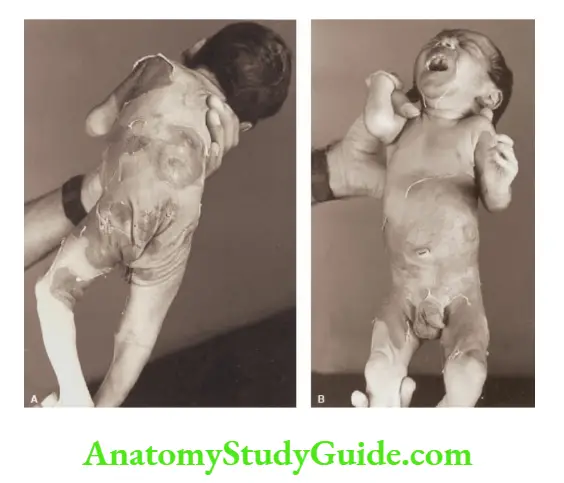
Bullae When vesicles are larger than 1.0 cm in diameter, they are called bullae. They may be intraepidermal or subepidermal.
Examples include epidermolysis bullosa and staphylococcal scalded skin syndrome. Cysts The circumscribed tumors containing semisolid or third contents are called cysts.
The typical examples are epidermal cysts that occur after puberty on the face and upper back, dermoid, sebaceous cysts, and branchial cysts.
Pustules The elevated well-circumscribed skin lesions containing purulent material or pus are called pustules.
Unlike the transparent dew drop appearance of vesicles, the pustules may be turbid or opaque and white or yellow in color.
Examples include folliculitis or pyoderma. Callus Localized hyperplasia of horny layer on the palm or sole due to pressure.
Comedones These are characteristic skin lesions of acne due to dark horny keratin and sebaceous plugs which are distributed on the face and upper back.
Open comedones or blackheads are 2–5 mm flesh-colored papules with black centers.
The closed comedones or whiteheads are 1–3 nun flesh-colored papules with a pinpoint opening. Petechiae Pinhead-sized macules of extravasated blood.
They cannot be blanched on pressure. Purpura The leakage of blood in the skin is called purpura or ecchymosis.
Unlike erythematous macules, purpura cannot be blanched by pressure with a finger or with a glass slide or a transparent plastic spatula (diascopy).
Petechiae are small, pinpoint areas (<3 mm) of hemorrhages while ecchymoses are large areas of extravasation of blood in the skin.


Ecchymotic skin patches may be flat or raised above the surface when there is associated vasculitis, viz. Henoch-Schönlein purpura and collagen vascular or connective tissue disorders.
Hematoma Swelling with or without fluctuation due to gross bleeding under the skin.
Telangiectasia Dilatation of superficial blood vessels which can be blanched by pressure.
Burrows, are linear, curved, or serpentine elevations or tunnels in the superficial skin produced by the adult female mite as she travels through the stratum corneum.
There is a black dot at the leading edge of the tunnel due to the lodgement of mites. Burrows are typically located
in the interdigital areas of palms and soles.
The primary skin lesions enable classification into broad groups of skin disorders which is useful for consideration of differential diagnosis.
The broad groups of primary skin lesions include maculopapular, papulosquamous, vesiculobullous, tumor nodules, vascular reactions (urticaria, purpura), eczematous, and pigmentary changes.
Secondary Skin Lesions
They are produced due to changes caused by scratching, touching, secondary infection, and because of local and systemic effects of medications.
Scales Desquamation or shedding of excess of the normal and abnormal horny layer of skin.
Crusts are formed by drying blood, serum, and any exudate overlying the diseased skin. They are often present in impetigo, in which they appear honey-colored and in weeping eczematous lesions.
Excoriations They develop as a result of linear loss of skin secondary to self-induced scratching and rubbing. Common examples include contact dermatitis, atopic dermatitis, and insect bites.
Erosions There is a partial loss of the epidermis which heals without scarring. Ulcers They occur due to deeper loss of the skin involving both the epidermis and a variable depth of dermis or subcutaneous tissue.
They may result from infection, vascular insufficiency, or burns. Eschar It is a necrotic skin lesion covered with a black crust.
Fissures They are linear clefts that are located deep in the epidermal layer in thickened or chronically inflamed skin.
Lichenification Thickening and hyperpigmentation of skill with exaggeration of skin markings due to chronic rubbing because of allergic or infective skin lesions are called lichenification.
Atrophy of the skin refers to the loss or thinning of the epidermis or dermis. Epidermal atrophy is characterized by wrinkling of the skin with telangiectases.
In dermal or subcutaneous atrophy, the skin is depressed. Eczematous skin lesions refer to inflammatory skin lesions which have indistinct margins with erythema and vesiculation in the acute phase.
Scaling, crusting, and lichenification may be seen as the disorder progresses.
Striae Atrophic pink or white linear skin lesions over the abdomen and buttocks due to alterations in the connective tissue because of sudden changes in tire girth as a result of obesity, pregnancy, and ascites.
Hyperkeratosis It is a histologic term used to describe the thickening of the stratum corneum. The presence of thick rough scales over skin lesions is a good clinical marker of hyperkeratosis.
Scar Healing occurs by replacement with fibrous tissue. When the formation of a scar is excessive, it is called a keloid.
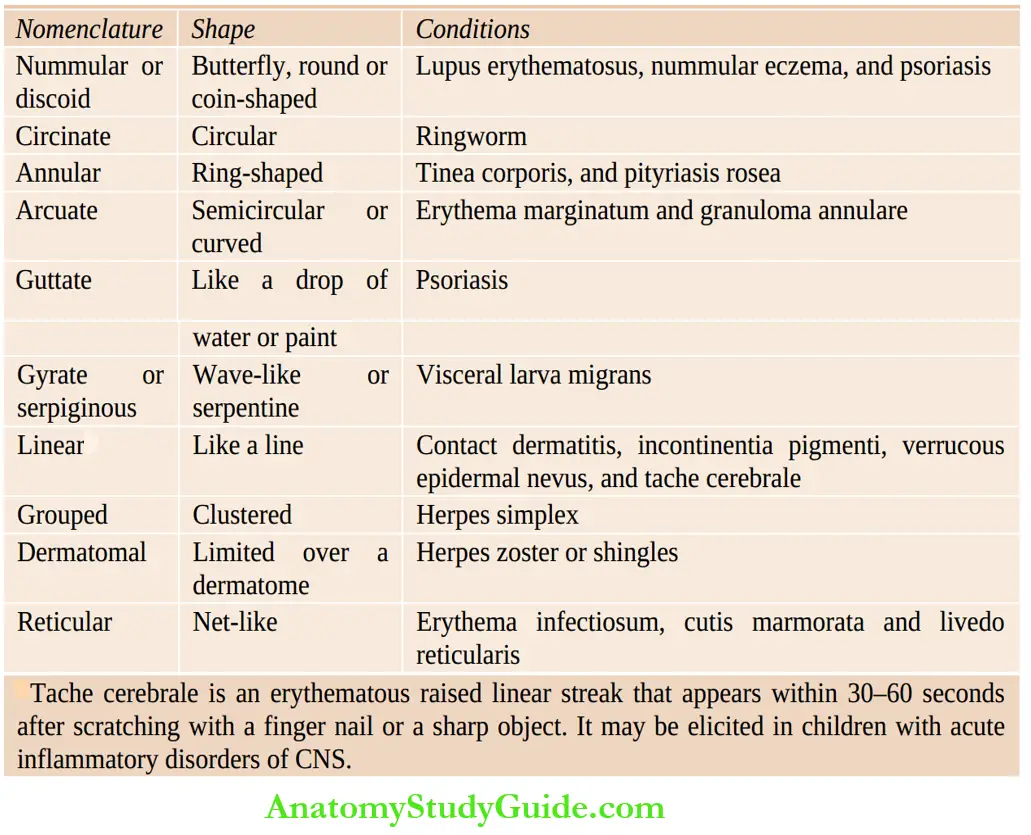
Morphology Of Skin Lesions
The configuration of skin lesions may provide useful diagnostic clues (Table 9.3). Linear lesions occur in a line and are characteristically seen in contact dermatitis and incontinent pigment.
Tache cerebral is an erythematous raised linear streak that appears within 30 to 60 seconds after scratching with a fingernail or a sharp object (Darier’s sign).
It may be elicited in patients with encephalitis, meningitis, and other acute CNS inflammatory diseases. Annular or ring-shaped lesions are seen in children with ringworm (tinea corporis), pityriasis rosea, and nummular eczema.
Semicircular or arc-like (arciform) lesions are suggestive of erythema marginate. The grouped lesions are called herpetiform lesions and are seen in herpetic infections.
Reticulated eruptions give a net-like or interlacing pattern as seen in patients with erythema infectious and incontinent pigment.
A number of other descriptive terms are used that often connote a specific disease entity.
For example, discoid (disk-shaped) usually refers to discoid lupus erythematosus, nummular (coin-shaped) is a type of eczema, and guttate (drop-like) refers to a form of psoriasis.
The lesions of lichen planus are slightly raised, flat-topped, and have a violaceous hue.
Distribution Of Skin Rash
The distribution of skin lesions should be carefully examined and may provide useful diagnostic clues.
When skin lesions are symmetrical in distribution, they are suggestive of endogenous causes while asymmetrical lesions may occur due to external factors.
Flexor distribution of symmetrical skin lesions is suggestive of atopic dermatitis while extensor distribution is seen in psoriasis.
Flexural distribution of rash occurs in a number of other conditions.
In chickenpox and pityriasis rosea, skin lesions are centripetal (over trunk) while in erythema multiforme and erythema nodosum, they are centrifugal (over extremities) in distribution.
In scabies, the face is characteristically spared (except in infants) and lesions are mostly concentrated over the interdigital areas of palms and soles and genital region.
Flexural distribution of skin rash
- Atopic dermatitis
- Infantile suborrheic dermatitis
- Intertrigo
- Candidiasis
- Tinea cruris
- Ichthyosis
- Inverse psoriasis
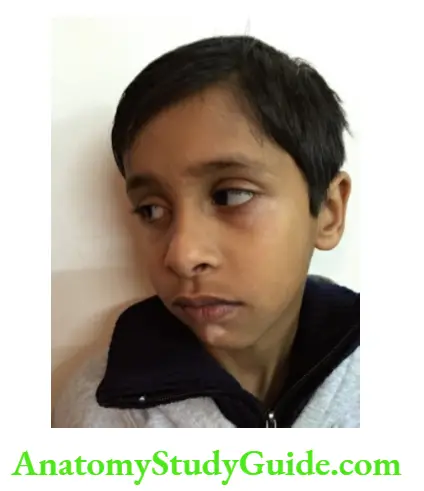
The presence of a rash on the face may provide a diagnostic clue to the underlying collagen vascular disorder.
Systemic lupus erythematosus is characterized by a typical sunlight-sensitive butterfly rash over the cheeks with marked erythema and papulovesicular lesions.
Heliotropic or lilac discoloration of the eyelids with periorbital edema is highly suggestive of dermatomyositis.
In addition, there is scaly erythematous dermatitis over the bony prominences, such as metacarpophalangeal, proximal interphalangeal joints, knees, elbows, and medial malleoli.
Erythema of palms and soles with or without desquamation is a recognized feature of prolonged steroid therapy, rheumatoid arthritis, hepatocellular failure, scarlet fever, hand-foot and-mostly disease, Kawasaki disease, and Rocky Mountain spotted fever.
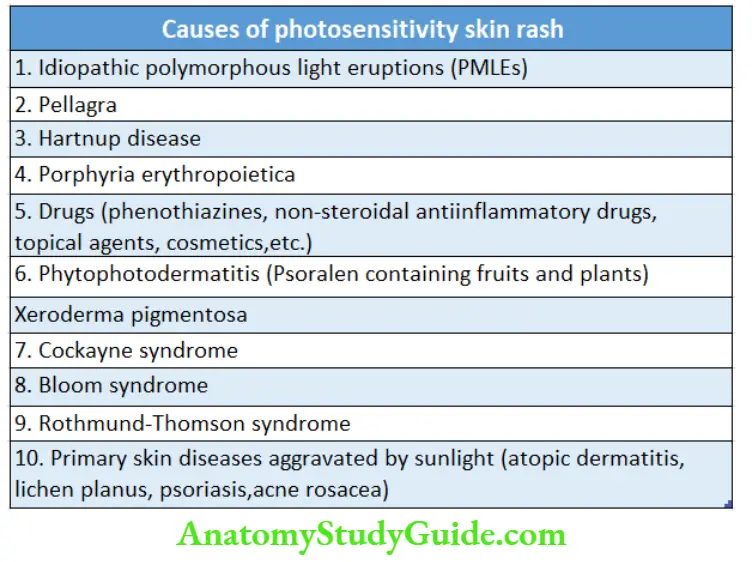
Skin rash over the exposed parts of the body (face, extremities, hands, and feet) due to photosensitivity is a characteristic feature of a number of disorders.

Color Of Skin Lesions
Macular erythematous skin lesions are most common. They occur due to viral exanthems as a result of dilatation of superficial cutaneous blood vessels.
Erythema readily blanches on pressure. Purpuric skin lesions do not blanch on pressure and they undergo color changes from bright pink to bluish-pink, blue, and dark brown over several days.
Petechiae and ecchymoses may occur due to thrombocytopenia, vasculitis, and life-threatening viral, bacterial, and treponemal infections.
The skin lesions may heal by desquamation and become lighter in color (hypopigmentation) after healing and recovery.
Depigmentation refers to total loss of pigment secondary to an autoimmune disorder (vitiligo) or due to hereditary disorders, like partial (piebaldism) and complete albinism, bi leprosy, skin lesions may be depigmented or reddened with a slightly raised edge and they may be anesthetic to pin-prick testing.
The cafeé-au-lait spots should be differentiated from NeoCell nevus by irregular borders and lighter color.
Pigmentation of lips is a feature of Peutz-Jeghers syndrome which is characterized by multiple polyps of the stomach or colon.
Dark brown or black pigmentation of extremities at friction sites (knuckles) and buccal mucosa is a characteristic feature of Addison’s disease.
Carotenemia produces orange-yellowish discoloration of skin akin to jaundice but there is no discoloration of sclera.
Livedo reticularis, a web-like pattern of reddish-blue discoloration mostly involving the legs, is seen in autoimmune vasculitis.
Vascular Nevi
Vascular birthmarks are hamartomas or benign tumor-like malformations composed of an admixture of vascular components. They may be visible at birth or appear later in infancy.
birthmarks are classified as flat (macular) nevi or elevated (papular, nodular, or tumor-like). They may spontaneously regress (involuting type) or persist throughout life (non-involuting type).
Flat Vascular Nevi
Involuting Type
Salmon patch (nevus simplex)
They are most common and found in almost 40 percent of neonates. They present as dusky pink blanching macules over the eyelids, glabella, forehead (angel kiss), and nape of the neck (stork bite).
They invariably fade away during infancy, except nuchal erythemas which may persist much longer.
Spider nevus (nevus araneus)
It is a small telangiectatic lesion consisting of a central arteriole from which superficial blood vessels radiate out. The radiating vessels collapse when the central punctum is pressed.
Cutis marmorata telangiectasia congenita (congenital phlebectasia)
It produces a mottled, marbled pattern of blue or dark-red erythema usually on an extremity.
The skin overlying the lesions is depressed, unlike livedo reticularis. It should be distinguished from symmetrical mottling of skin following exposure to cold which is a transient vasomotor phenomenon.
Non-involuting Type
Port-wine stain (nevus flammeus)
It presents as dark-red or purple-red macules on the face, neck, or extremities with unilateral and segmental distribution.
The presence of port-wine stain over the face affecting the skin innervated by the ophthalmic branch of the trigeminal nerve may be associated with Sturge-Weber syndrome (ipsilateral glaucoma and leptomeningeal cerebral calcification due to meningeal angiomatosis).
Nevus flammeus is a recognized component of Klippel-Trenaunay-Weber syndrome, Parkes-Weber syndrome, hyperkeratotic capillary-venous malformation, Proteus syndrome, Rubinstein-Taybi syndrome, Beckwith-Wiedemann syndrome and trisomy-13.
Raised Vascular Nevi
Involuting Type
Hemangioma of infancy (strawberry nevus, cavernous hemangioma)
The typical lesion is dark- or bright red like a strawberry raised above the skin surface and compressible on pressure.
They may be absent or small at birth and initially enlarge in size as the child grows. They may ulcerate, bleed or compromise the functioning of a vital organ.
After one year, the involution starts from the center of the lesion which becomes pale and atrophic.
When cavernous hemangiomas are multiple or deep-seated, they may be associated with high-output cardiac failure or disseminated intravascular coagulation (Kasabach-Merritt syndrome) because of the trapping of platelets.
The deep-seated lesions should be differentiated from arteriovenous malformation which may be warm to touch and usually has a thrill or bruit and diagnosis can be confirmed by Doppler sonography.

Non-involuting Type
Pyogenic granulomas and lymphangiomas are classified in this group but they are not truly vascular nevi.
Lymphangioma produces a skin-colored, ill-defined mass of lymphatics that hangs loosely, is compressible and transilluminate, and feels like a bag of worms. They do not regress and are managed by surgical excision.
Warts
Warts are caused by more than 200 types of human papillomaviruses (HPV). The virus enters the skin through breaks in the epithelium and causes hyperplasia of the squamous epithelium.
Warts are well-circumscribed papules with an irregular, roughened, keratotic surface. Common warts are skin-colored, rough, minimally scaly papules and nodules found on the exposed surfaces of the hands, face, arms, and legs.
Flat warts occur in clusters over the hands, arms, and face. Periungual and plantar warts may be painful and occur due to inward-growing hyperkeratotic plaques and papules.
Anogenital warts occur in sexually active adolescents as a result of infection with HPV types 6 and 11.
They are characterized by moist, fleshy, papillomatous lesions on the perianal mucosa (condylomata acuminate), labia, vaginal introitus, perineal raphe, and on the shaft, carona, and glans penis.
Molluscum Contagiosum
It is caused by a pox virus which is a large double-stranded DNA virus that replicates in the cytoplasm of host epithelial cells.
The skin lesions are discrete, pearly, skin-colored, smooth, dome-shaped papules varying in size from 1–5 nun. They are characterized by central umbilication from which a plug of cheesy material can be expressed.
The papules may occur anywhere on the body but the face, eyelids, neck, axillae, and thighs are commonly affected. The
lesions may be large in size or widespread in immune-deficient children.
Neuroectodermal Dysplasias
Skin and central nervous system are both ectodermal in origin and the presence of ectodermal dysplasias is a good marker of associated CNS abnormalities and seizures.
Most of these diseases are inherited as autosomal recessive disorders except ataxia telangiectasia which is a dominant condition. They are summarized in.


Appendages Of Skin
Hair and nails provide protection to the skin and have a common embryologic origin or background. Many developmental or acquired skin disorders may have associated abnormalities in the hair, nails, and teeth.
Nails may be absent in inherited nail-patella syndrome. Splinter hemorrhages under the nail bed may occur due to trauma, psoriasis, collagen vascular disorder, bacterial endocarditis, and trichinosis.
Several acquired disorders of the skin are associated with abnormalities in the mucous membranes, hair, and nails.
Anhidrotic ectodermal dysplasia is characterized by hyperthermia (fever due to the rise of environmental temperature because of the absence of sweat glands), alopecia, and the absence of eyebrows and eyelashes.
Hypertrichosis or excessive generalized growth of body hair over the non-sexual areas of the body is seen in a number of systemic disorders.
Systemic conditions associated with hypertrichosis
- Familial or constitutional
- Drugs like corticosteroids, phenytoin, cyclosporine, and minoxidil
- Cushing syndrome
- Chronic malnutrition or starvation
- Porphyria curtana tarda
- Coffin-Siris syndrome
- Cornelia de Lange syndrome
- Treacher Collins syndrome (hair on the side of the face)
Hirsutism or androgen-related male pattern of hair growth on the face and pubis in adolescent girls is most commonly idiopathic as a racial or constitutional trait due to end-organ hypersensitivity to androgens.
The common causes of hirsutism are listed in. When there is androgen excess, libido is increased and menstrual cycles become irregular and scanty.
The presence of regular menstrual cycles is a piece of good evidence against significant androgen excess, suggesting that hirsutism is constitutional and not pathological.
The scalp should be examined for seborrhea, discoid lesions of tinea capitis and psoriasis, alopecia, pediculosis, and depigmentation.
The presence of an occasional grey scalp hair in a child is a cause for concern for some parents. It is of no clinical significance and is often ascribed to constitutional factors or chronic illness and nutritional disorders.
The presence of white forelock or piebaldism may be associated with sensorineural deafness (Waardenburg syndrome) and Hirschsprung disease (Shah-Waardenburg syndrome.) Rarely, hair may show alternate bands of depigmentation producing typical flag signs in children with kwashiorkor.
A number of systemic disorders are associated with sparse light-brown and brittle scalp hair. Many of these disorders are associated with a variety of skin manifestations.
Common causes of hirsutism
- Racial or constitutional
- Polycystic ovary disease (PCOD)
- Late-onset congenital adrenal hyperplasia
- Androgen-secreting ovarian or adrenal tumor (Cushing syndrome)
- Acromegaly
- Intake of androgens, progestogens, and corticosteroids
Causes of sparse, light-brown, and brittle scalp hair
- Kwashiorkor
- Cretinism
- Chronic debilitating disease
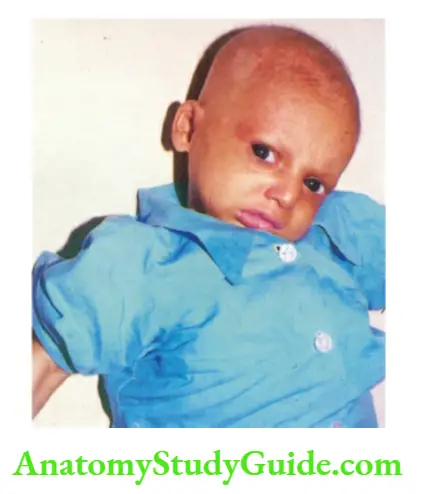
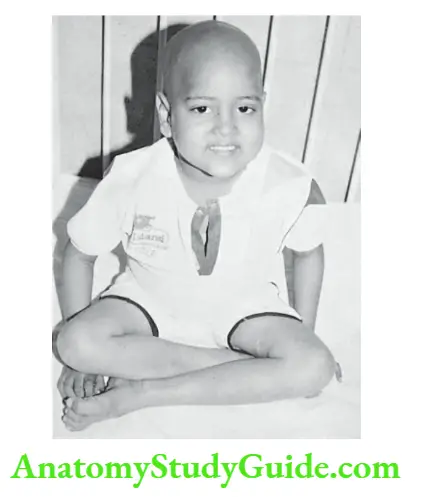
- Progeria
- Ectodermal dysplasia
- Hypervitaminosis A
- Acrodynia
- Adrenal insufficiency
- Cartilage-hair hypoplasia syndrome
- Langer-Giedion syndrome
- Hallermann-Streiff syndrome
- Trichotillomania (a ball of hair or trichobezoar due to swallowed hair may cause obstruction in the stomach)
- Trichorrhexis nodosa (‘paint-brush hair)
- Incontinentia pigmenti
- Conradi disease
- Congenital syphilis
- Idiopathic hyperparathyroidism
- Zinc deficiency
- Copper deficiency
- Acrodermatitis enteropathica
- Biotinidase deficiency
- Anorexia nervosa
- Homocystinuria
- Menke’s syndrome (Kinky hair disease)
- Alopecia areata (No hair follicles with typical ‘exclamation mark’ hair over the bald area)
- Traction alopecia (‘pony-tail’ alopecia)
- Tinea capitis
- Coffin-Siris syndrome
- Polyendocrine deficiency
- Scarring alopecia (burns, severe infections, lichen planus, systemic lupus erythematosus, herpes zoster
- Drug-induced
Pitting of nails along with thickening, loss of luster, and subungual keratosis may occur in psoriasis, atopic dermatitis, and onychomycosis.
White spots or vertical lines in the nails (leukonychia) may be caused by trauma, nutritional deficiency, and chronic debilitating disorders.
Dystrophic nails are a recognized feature of epidermolysis bullosa, ectodermal dysplasia, chondroectodermal dysplasia, and nail-patella syndrome.
Dysplasia of nails is seen in infants with fetal alcohol and phenytoin syndromes. Tuberous sclerosis may have associated subungual and periungual fibromas arising from the groove of the nail beds of fingers and toes.
Common Skin Conditions
There are a number of relatively common and some unusual skin conditions which should be identified by the primary physician and pediatrician.
Most dermatological conditions are diagnosed on the basis of morphology and distribution of skin lesions. The salient diagnostic clinical features are given below. The list is merely representative and in no way exhaustive.
Acne Vulgaris
It is a chronic inflammation of the pilosebaceous units due to the excessive production of androgens during adolescence and puberty.
The common predisposing factors include genetic predisposition, sex hormones, emotional stress, and intake of certain drugs (corticosteroids, hydantoin, lithium).
Seborrhea of the scalp and face due to excessive secretion of sebum may coexist. Microbial colonization (Propionibacterium acnes) and occlusion of pilosebaceous orifices with keratin plugs lead to a perpetuation of lesions.
The disorder is more severe in males, while it is more protracted in females. The sites of predilection of skin lesions include the face, neck, upper arms, shoulders, and back.
A variety of skin lesions, like papules, nodules, and cysts may occur.
The characteristic skin lesions are open comedones, 2–5 mm flesh-colored papules with black plugs of keratin (blackheads).
The closed comedones or white heads are 1–3 mm fleshcolored papules with pinpoint openings.
Superadded bacterial infection and unnecessary squeezing of comedones or nodules may lead to the formation of scars which may be atrophic (pitted scars) or hypertrophic (keloids).
Scabies
It is a contagious disease caused by the bites of a mite Sarcoptes scabie var. hominis.
The characteristic skin lesions include linear or S-shaped burrows with black dots at the leading edge mostly over the axillae, beltline, flexor surfaces of extremities especially wrists, interdigital areas of palms and soles, and genital region.
Due to hypersensitivity reactions to the mites and their products, the intensely pruritic papular or papular-vesicular rash develops over the lower abdomen, buttocks, axillary folds, and groins.
The face is usually spared except in infants. There is intense and intractable itching, especially at night.
There are secondary excoriations, eczematous areas, pustules, and crusting as a consequence of itching, rubbing, and secondary infection. The disease is highly contagious and several family members are affected simultaneously.
Atopic Dermatitis
The distribution of skin rash in atopic dermatitis varies depending on the age.
In infancy, cheeks, wrists, and extensor surfaces of the arms and legs typically develop papulovesicular, often weeping or wet lesions, which may develop fine scabs or lichenification.
The scalp and postauricular areas are often affected while the diaper area is usually spared. Secondary infection and traumatic lesions may develop due to scratching and rubbing.
In older children, dry maculopapular lesions are mostly distributed over the flexor surfaces of extremities, neck, wrists, and ankles.
Xerosis and lichenification commonly supervene, hi a number of disorders, skin rash is distributed over flexural surfaces. Eosinophilia and elevation of serum IgE levels provide useful laboratory support to the diagnosis.
Wiskott-Aldrich syndrome (WAS) is a rare X-linked disorder characterized by eczema, thrombocytopenia (reduced number as well as size of platelets), immune deficiency, and bloody diarrhea.
These infants are prone to develop autoimmune disorders.

Seborrheic Dermatitis
Seborrheic dermatitis is usually associated with seborrhea capita (dandruff) and has a predilection for infants and adolescents.
The condition starts from the scalp with greasy-yellowish scales and extends down the forehead to involve the eyebrows, nose, and ears.
Intertriginous areas and diaper areas may be affected due to superadded Candida infection. Loss of scalp hair and depigmented skin lesions are seen dining the course of the disease.
The clinical differentiation from atopic dermatitis may be difficult at times. The absence of eosinophilia and normal serum IgE levels support the diagnosis of seborrheic dermatitis.
Papular Urticaria
It is a common, intensely pruritic disorder caused by an allergic response to insect bites. The fresh lesions are papules with a punctum on an erythematous base mostly distributed over the exposed areas of the skin.
Most cases occur during summer and spring due to mosquito and flea bites. Excoriations and secondary infection may lead to hyperpigmentation in older lesions.
Nutritional Disorders
Zinc deficiency (Acrodermatitis enteropathica) Skin manifestations are characteristically seen around the perioral, periorbital, and perianal areas.
Distal parts of limbs especially hands and feet also develop skin manifestations. The vesiculobullous skin lesions soon become dry, scaly, and crusted with sharply demarcated borders.
The vesicles rapidly rupture, revealing a moist, red base that subsequently dries and becomes plaque-like. Diarrhea and alopecia are commonly associated.
Affected infants are irritable, listless, and fail to thrive. Essential fatty acid deficiency It is characterized by generalized scaly dermatitis composed of thickened, erythematous, desquamating plaques.
Alopecia, thrombocytopenia, and failure to thrive are often associated.
Skin Lesions with Fine Scales
Pityriasis alba It is a common, asymptomatic skin condition of unknown etiology (possibly due to S. albus) in infants and young children. The lesions are more common in summer and following exposure to sunlight.
The skin lesions are well-demarcated hypopigmented round or oval patches with minimal fine lamellar or branny scales.
The lesions, 1–3 in number, most commonly occur on the face but may be present on the neck, upper trunk, and proximal parts of limbs.
Pityriasis or tinea versicolor It is characterized by the appearance of asymptomatic ovoid or coin-shaped brown-colored or whitish macules over the neck, chest, and back.
The lesions have fine branny scales (pityriasis means “bran-like” scales) which can be easily scraped off with the edge of a glass slide. Pruritus is usually absent or minimal.
Most cases occur after puberty during hot and humid summer months. KOH preparation may show characteristic round and elongated cells of M. furfur.
Pityriasis rosea is a common disorder of unknown etiology usually seen in adolescent children and young adults.
There is some evidence that the disease may have a viral etiology because it is common in spring and autumn and one attack usually gives long-lasting immunity.
The rash may be preceded by mild constitutional symptoms, such as fever, headache, malaise, and arthralgia. In half the patients, there is an oval flesh-colored herald patch on the trunk measuring 1–10 cm in size.
It is usually present on the trunk as a round or oval patch with a central wrinkled salmon-colored area and a darker peripheral zone separated by a “collarette of scales”.
After a few days of herald patch, a generalized skin rash appears on the trunk. The eruption consists of oval flesh-colored or pink macules with central clearing and raised fine scaly edges.
The skin lesions are usually symmetrical and their long axis follows lines of cleavage resulting in a pattern of Christmas or fur tree on the back.
Itching is minimal or absent. The disorder is often mistaken with tinea corporis and skin lesions at times are described as “lots of ringworms” by the young resident.
The eruption continues to evolve for about 2 weeks and skin lesions usually persist for 3 to 8 weeks and at times for several months.
Fungal Infections (Dermatophytoses)
Tinea capitis There are no characteristic features. It often presents as a kerion with an inflammatory, boggy, pustular patch with localized alopecia of the scalp.
The typical scaly circular lesion with raised edges and central clearing that is seen in tinea corporis is uncommon in tinea capitis.
There is the formation of scales, schematization, and scab formation. The condition should be differentiated from seborrheic dermatitis, pustular folliculitis, and trichotillomania.
The KOH preparation is not reliable in tinea capitis and diagnosis is best confirmed by fungal culture. tinea corporis It is characterized by annular erythematous ring lesions with active elevated margins and central clearing.
The border is generally scaly, slightly elevated, and often studded with microvesicles and tiny pustules. The lesions may be single or multiple.
Tinea corporis should be differentiated from herald patch of pityriasis rosea, granuloma annual, and dry nummular eczema.
Candida infection of the skin has a special predilection for moist areas like the diaper area, neck, axillae, groin, and perioral and perianal regions.
It produces confluent bright-red erythema with maceration and fissuring. There are vesicula-pustular lesions over the
edge or periphery of erythematous base as “satellite lesions”.
In candidiasis of the diaper area, deep areas of inguinal folds are invariably affected. Oral thrush and paronychia candidal infection may coexist.
Congenital cutaneous candidiasis is characterized at birth or within 12 hours of life by multiple erythematous macules or vesiculopustular lesions.
After the neonatal period, the development of recurrent or persistent candidiasis should alert the pediatrician to look for an underlying cell-mediated immunodeficiency disorder.
Miscellaneous Conditions
Drug Eruptions
Adverse cutaneous drug eruptions are common and range from transient maculopapular skin rash to Stevens-Johnson syndrome or even fatal toxic epidermal necrolysis (TEN).
The most common drug eruptions include maculopapular skin rash and fixed drug eruption.
Drug eruptions may occur following any medication but are most common during the administration of sulfonamides (co-trimoxazole), dapsone, antibiotics (especially penicillin and its derivatives), antiepileptics, and antitubercular drugs.
The Cutaneous drug eruption is characterized by the sudden appearance of skin rash during intake of drug(s), (Allopathic, Homeopathic, Ayurvedic, etc.), home remedies, or topical agents.
The skin rash is sudden or abrupt in onset, symmetrical in distribution (except in fixed drug eruption) and often pruritic.
The morphology of the rash may be exanthematous (erythematous, macular, maculopapular), urticarial, or vesicular.
The skin eruption resolves on withdrawal of the drug and would reappear when the same or a similar drug is given again to the patient. In immune-mediated drug eruptions, there may be eosinophilia or elevation of IgE antibodies.
In any patient with sudden onset of skin eruption, adverse cutaneous drug reactions must be considered, if a child is receiving medications.
Fixed drug eruptions are uncommon in children but manifest characteristic skin lesions which recur at fixed sites on reexposure to the drug.
There are single or multiple circular or oval erythematous macule(s) or plaque(s) with burning or tingling sensations. They are commonly located at the mucocutaneous junctions and leave behind slate-gray-colored pigmentation on healing.
Phrynoderma (Toad Skin)
Phrynoderma is a type of follicular hyperkeratosis that is typically distributed over the extensor surfaces of elbows, knees, anterolateral thighs, and buttocks.
The morphology of skin lesions is variable and may range from filiform papules to small conical papules to large papules with horny puncta.
Generalized xerosis with fine wrinkles and scales may be present. Phrynoderma is a typical manifestation of vitamin A deficiency but it may be associated with deficiencies in vitamin B complex, vitamin C, vitamin E, and essential fatty acids.
The condition should be differentiated from keratosis pilaris and Darier’s disease.
Erythema Multiforme
It is characterized by erythematous lesions of pleomorphic morphology over the extremities. The lesions begin as erythematous macules and evolve into papules, vesicles, bullae, urticarial plaques, or patches of confluent erythema.
The pathognomonic lesions of erythema multiforme are iris or target-shaped lesions which have a dusky center, an inner pale ring, and an erythematous outer border.
The symmetric crops of skin lesions usually occur on extensor surfaces of arms and legs often involving palms and soles.
The skin lesions may heal over 4–6 weeks with hypopigmentation or hyperpigmentation but without any scarring.
When skin lesions are associated with the involvement of two or more mucous membranes, the condition is called Stevens-Johnson syndrome.


Lichen Planus
Lichen planus (LP) is a papulosquamous disorder characterized by pruritic, polygonal-shaped, flat-topped, shiny, violaceous papules.
Examination with a hand lens may reveal a network of gray lines (Wickham’s striae). The skin lesions have a special predilection for the involvement of wrists, shins, lower back, and genitalia.
Involvement of the scalp may lead to hair loss. The buccal mucosa is commonly involved leading to white net-like reticular eruption.
Koebner’s phenomenon may be present, i.e. the lesions may be induced in areas of local injury, such as scratches. The etiology of LP is unknown but it may be immunologically mediated with genetic predisposition.
Its course is variable but most patients have spontaneous remission within 6 months to 2 years. Topical steroids provide symptomatic relief.
Granuloma Annulare
It is an uncommon chronic skin disorder affecting school-going children and young adults. It is characterized by the appearance of semilunar or arciform flesh-colored or pink smooth papules.
The lesions coalesce to assume an oval, round, or ring-like shape with a central clearing. The size of lesions varies between 1 and 5 cm, single or multiple, and may occur anywhere on the body but most commonly over the extremities.
The skin lesions are smooth, without any scales or epidermal involvement. The lesions are asymptomatic and may take a few months to 2 years to resolve spontaneously.
The absence of epidermal involvement, lack of scales, and multiple lesions without itching differentiate granuloma annual from tinea corporis.
Vitiligo
It is characterized by the development of depigmented patches of skin due to dysfunction or destruction of melanocytes possibly because of an autoimmune mechanism.
There is an increased association with other autoimmune disorders, like thyroiditis, adrenal insufficiency, pernicious anemia, polyendocrinopathy, and mucocutaneous candidiasis.
Family history may be positive in one-third of patients.
Skin lesions are usually oval in shape and form various geographic patterns with scalloped margins, hi dark-skinned subjects, the patches assume milky-white or snow-white color.
The distribution of skin lesions may be generalized and symmetrical or limited to a segment of the trunk or limb.
The lesions are more likely to occur at the sites of repeated trauma (ankles, elbows, knees) or scratching (Koebner phenomenon).
The distribution of lesions at the edges or around the eyes, nose, and lips is characteristic of vitiligo. Depigmentation or graying of hair, choroid, and retina (chorioretinitis) may be associated
Psoriasis
It is a genetically determined, inflammatory, and proliferative disorder of the skin because of unknown etiology.
It is a chronic disorder characterized by the appearance of sharply demarcated, all-red, or salmon-colored papules and plaques covered with silvery-white scales.
When attempts are made to remove the scales, there is oozing of minuscule droplets of blood (Auspitz phenomenon).
Skin lesions may occur at any site but are more common over the elbows, knees, intertriginous areas, and scalp. The lesions over the palms and soles may become pustular.
Rarely generalized erythrodermic psoriasis may be seen in infants. The skin lesions are aggravated by the intake of certain drugs (oral corticosteroids, lithium, beta-blockers, chloroquine, alcohol), exposure to sunlight, stress, and obesity.
There may be involvement of nails leading to pitting, subungual hyperkeratosis, and yellowish-brown spots under the nail plate (oil spots). Psoriatic arthropathy is uncommon in children.
Graft-Versus-Host Disease (GVHD)
The acute form of GVHD manifests with maculopapular rash (which may progress to toxic epidermal necrolysis in a fulminant case) with diarrhea, tachypnea, and hepatosplenomegaly.
The chronic form of GVHD is characterized by hyperkeratotic skin rash, hepatosplenomegaly, hair loss, chronic diarrhea, and wasting.
Toxic Epidermal Necrolysis (TEN)
It is characterized by the loosening of large sheets of the epidermis with the formation of flaccid bullae. The bullae rupture leads to exposure of intensely pink, underlying epidermis or dermis which gives an appearance of scalded skin.
Nikolsky sign is positive, i.e. epidermis can be readily peeled off by rubbing the skin at the normal sites. Other conditions with positive Nikolysky signs include pemphigus vulgaris and staphylococcal scalded skin syndrome.
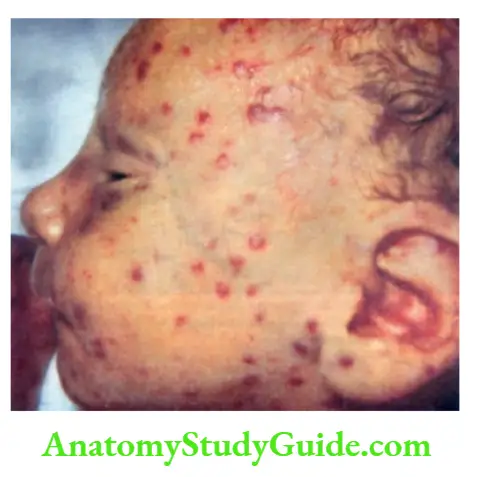
TORCH Infections
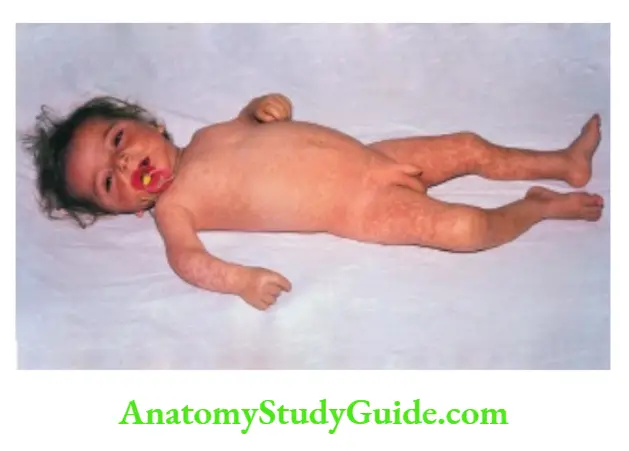
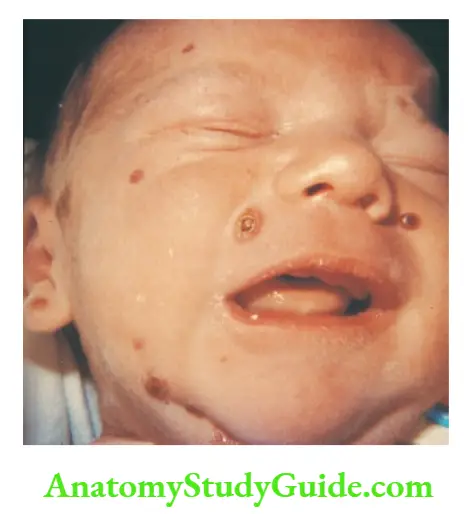
Intrauterine infections may show manifestations of petechiae and ecchymoses over the trunk and extremities due to thrombocytopenia.
“Blueberry muffin” spots are discrete, well-circumscribed skin lesions due to dermal erythropoiesis in severely affected infants with congenital CMV infection.
Congenital syphilis is characterized by maculopapular skin rash initially oval and pink but subsequently turns coppery brown with desquamation, especially over the palms and soles.
A characteristic vesiculobullous eruption with erythema, blister formation, and crusting may occur over the extremities, palms, and soles.
Acrodermatitis Enteropathica
It is a rare autosomal disorder of zinc transport due to a defective gene winch mapped to 8q24. Breast milk contains a compensatory zinc-binding ligand that facilitates the absorption of zinc.
The manifestations start after 1–2 weeks of weaning from breastfeeding.
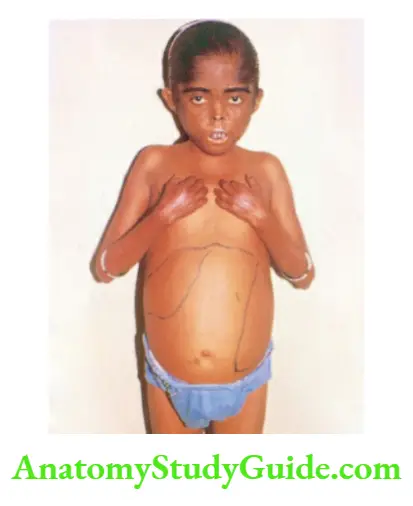
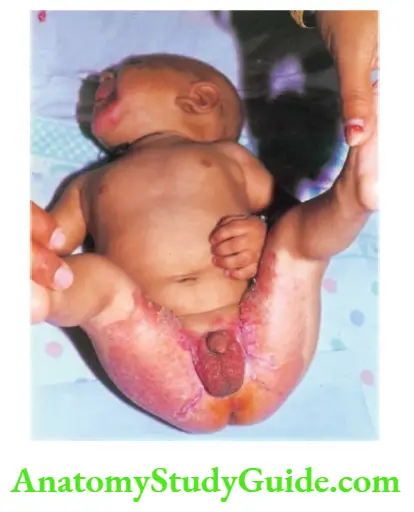
It is characterized by eczematous scaly skin rash winch becoming vesicular, bullous, pustular, or desquamative, involving peripheral or acral parts of the extremities, perioral and anogenital areas.
Angular cheilitis (perleche) is a common early manifestation followed by paronychia.
It is usually associated with intractable diarrhea, graying of hair, progressive alopecia, and superadded infection with bacteria and Candida albicans.
Acrodermatitis enteropathica is characterized by a triad of acrodermatitis with a special predilection for body orifices, diarrhea, and alopecia.
The condition should be differentiated from severe seborrheic dermatitis, deficiency of essential fatty acids and biotin, and methylmalonic acidemia.
Cutaneous Tuberculosis
Mycobacterium tuberculosis can affect any organ of the body. The skin manifestations depend upon the immunity of the patient and the route of inoculation.
The diagnosis is confirmed by the isolation of acid-fast bacilli and histopathology. Lupus vulgaris It is characterized by a solitary well-demarcated reddish-brown plaque on the head, neck, and thighs.
When the lesion is pressed with a glass slide or transparent spatula (Diascopy), apple jelly nodules are visible.
During recovery, the center becomes atropine and scarred with the development of nodules. Scrofuloderma The skin is involved by contiguous inoculation from tubercular lymph node(s)(usually cervical), bone (tibia), or joint (sternoclavicular).
There is a chronic discharging ulcer with non-healing everted edges.
Tuberculous verrucous cutis It is a rare manifestation of cutaneous tuberculosis which is characterized by a solitary firm and warty plaque with a violaceous halo and central scarring.
Hansen Disease
Hansen disease or leprosy is a chronic granulomatous disease affecting the skin and peripheral nerves. The disease has a long incubation period (usually >6 months) and is caused by Mycobacterium leprae.
Skin lesions consist of macules, plaques, and nodules which are hypopigmented and erythematous with well-defined margins.
There is atrophy of the skin with loss of sweating and hair over the involved skin.
The patches are characteristically hyperesthetic or anesthetic due to the involvement of peripheral nerves winch become thickened and tender on palpation.
Demonstration of acid-fast bacilli from skin smear or biopsy material is diagnostic. Advanced cases develop sequelae, like trophic ulcers, deformities (saddle nose, claw hand, and toes, foot drop), and ophthalmological complications.
Leave a Reply