Temporomandibular Joint
The temporomandibular joint (TMJ) also called the craniomandibular joint is the synovial articulation between the mandibular fossa in the temporal bone and the movable condyle of the mandible. It is a synovial joint and has a joint cavity filed with synovial fluid and thus allows considerable movement of the joint. The synovial fluid is secreted by the synovial membrane and lines the internal surface of the capsule of the joint.
Table of Contents
Read And Learn More: Oral Histology Notes
Anatomy Of The Temporomandibular Joint
The temporomandibular joint (TMJ) is the articulation between the temporal bone in the skull and the mandible. It is a diarthrodial and ginglymoid joint of the synovial type. This is a complex bilateral joint between the skull and the movable mandible and has very high significance.
Functions Of The Temporomandibular Joint
- Important for speech articulation
- Mastication
- Various complex mandibular movements
Components Of The Temporomandibular Joint
Glenoid fossa:
- The concave articular surface of the temporal bone which is situated on the inferior surface that receives the condyle is the glenoid fossa.
- It is also referred as the mandibular fossa.
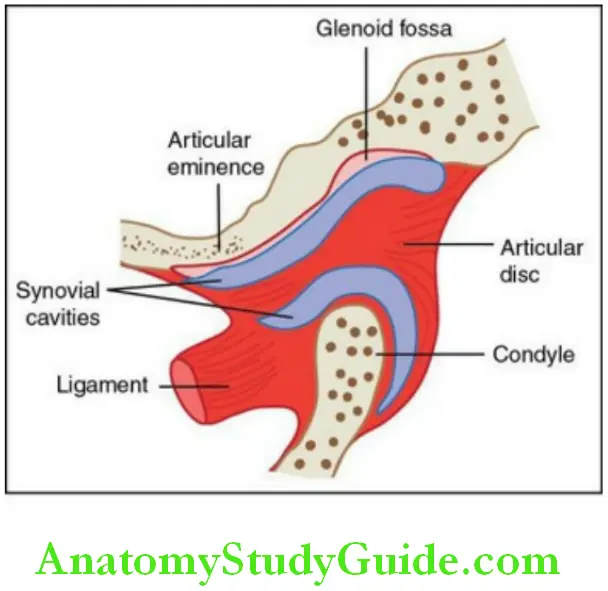
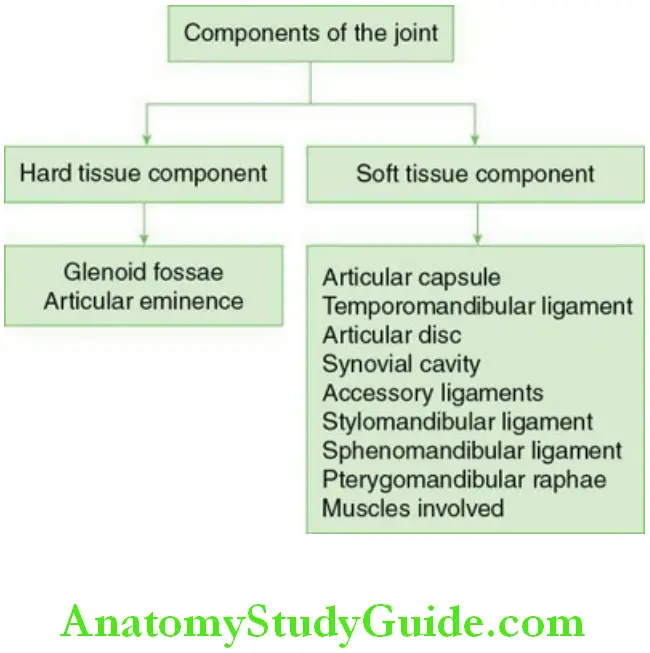
Articular eminence:
- The articular eminence is convex antero-posteriorly.
- The convex part of the temporal bone which is in the anterior region is called the articular eminence. It binds the mandibular fossa anteriorly.
- This is also called the articular tubercle and is enclosed by the articular capsule of TMJ.
Articular capsule:
- The thin sleeve of dense cartilaginous tissue enclosing the joint cavity is called the articular capsule.
- The capsule originates from the glenoid fossa and the anterior eminence and then attaches to the edges of the disc inserting around the rim of the condyle.
The anterolateral part of the capsule is thickened like a band to form the
temporomandibular ligament. - The synovial fluid is present in the upper and lower joint compartments.
- The articular capsule is responsible for holding the articular disc in place between the mandibular condyle and fossae. The capsule holds the joint from dislocation during excessive mouth opening.
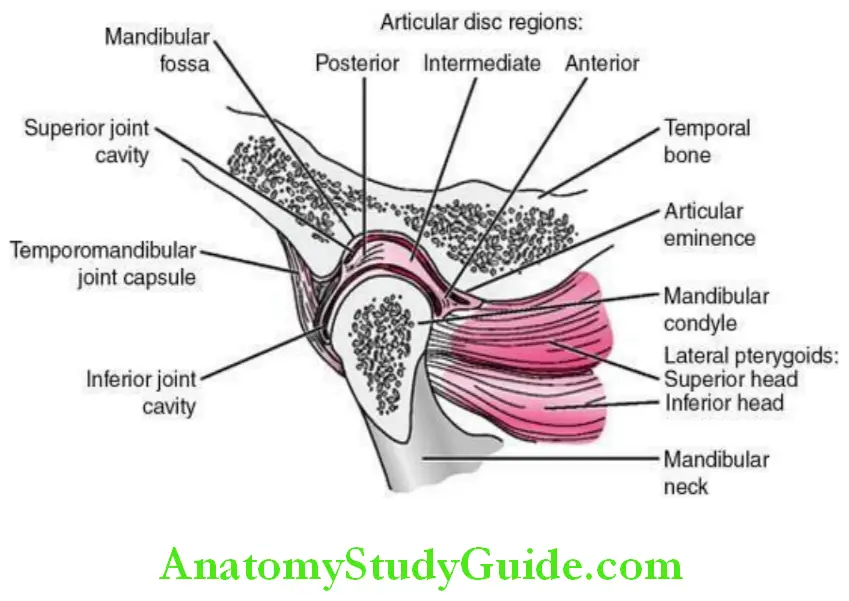
Articular disc:
- The interarticular disc is a biconcave flexible fibrous cartilage which is present between the condyle and glenoid fossae. It acts as a shock absorber during various mandibular movements.
- The superior and inferior heads of the lateral pterygoid muscle insert into the disc and the capsule. The upper part of the disc is concave which fits into the articular eminence and convex pertaining to the rest against the articular fossae.
Temporomandibular Joint Anatomy Synovial cavity:
During mouth opening, the condyle rotates and moves forwards into the articular eminence. The articular disc travels with the condyle forming a meniscus which divides the compartment into two synovial spaces filled with synovial fluid.
Mandibular ligaments:
The principle mandibular ligament is the temporomandibular ligament. The accessory ligaments are
- Stylomandibular ligament
- Sphenomandibular ligament
- Pterygomandibular raphae
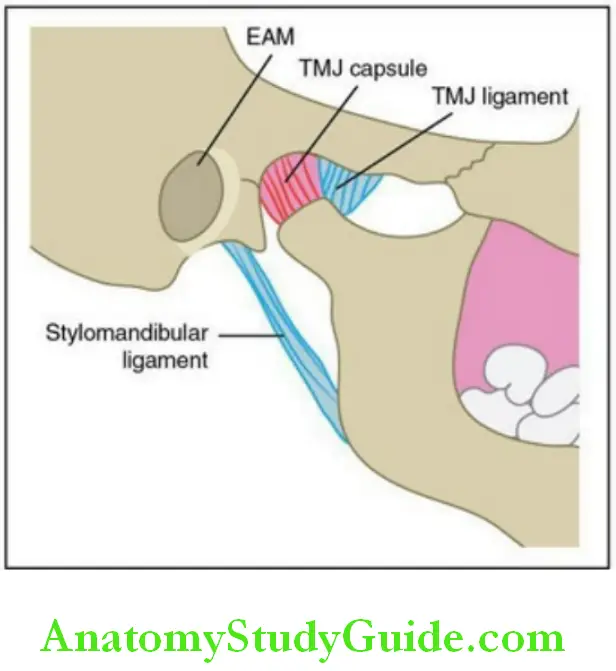
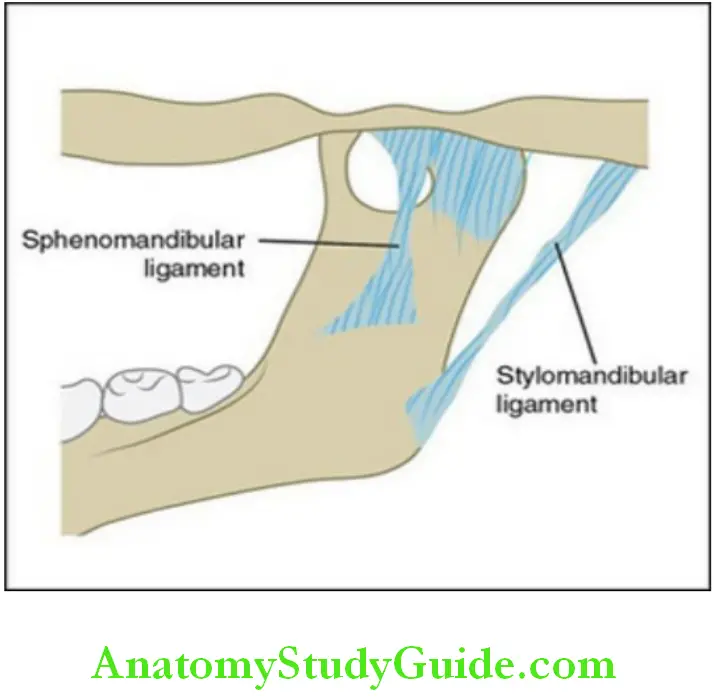
Stylomandibular ligament:
- The stylomandibular ligament extends from the styloid part of the stylomandibular temporal bone and inserts into the posterior border of the angle of the mandible between the masseter and internal pterygoid. This ligament helps during jaw movements.
Sphenomandibular ligament:
- The sphenomandibular ligament arises from the spine of sphenoid bone and from the petrotympanic fissures and inserts anterior superiorly to mandibular foramen in the lingula. This ligament is often passive during jaw movements.
Pterygomandibular raphae:
- The pterygomandibular raphae is a tendinous band of buccopharyngeal fascia which is attached by one extremity to hamulus of medial pterygoid plate and the other to the posterior end of mylohyoid line in mandible.
Mandibular Movements
Mandibular movements are complex in nature, which happen bilaterally and involve TMJ, muscles and ligaments. The movements occur in various angles and may not be symmetrical between the two joints. The basic understanding of the anatomy of the TMJ and its movements is necessary in diagnosing joint-related facial pain.
The factors controlling the mandibular movements are
- Condylar path
- Muscles of mastication
- Teeth contact
The three factors form a triad. There needs to be a balance and coordination between these three determinants for smooth functioning of the TMJ.
Temporomandibular Joint Anatomy – The different movements of the TMJ are:
1. Basic movement
- Rotation/hinge movement
- Translation
Rotation:
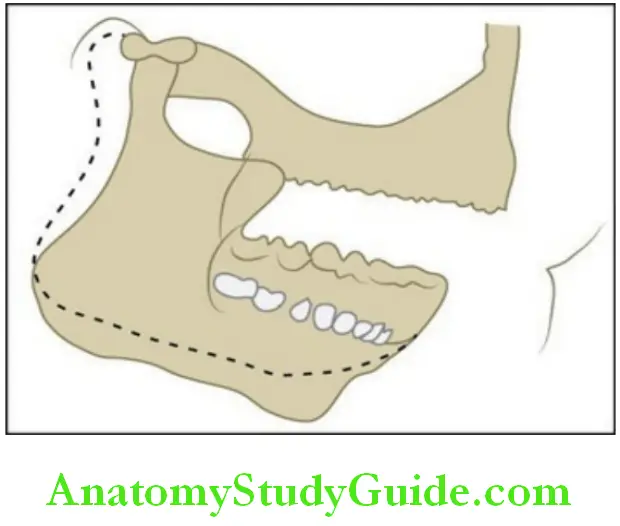
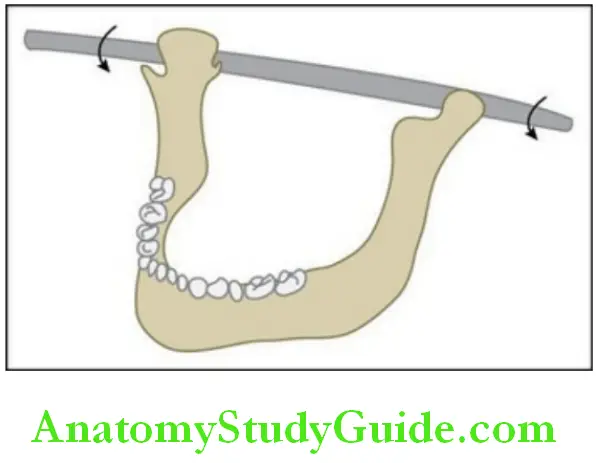
- Rotation is also called hinge movement, as the movement is like a door hinge. When the mouth is opened slightly (up to 12 mm), the mandibular condyle rotates within the joint without bodily displacement. The lower joint cavity allows the hinge movements.
Temporomandibular Joint Dysfunction Symptoms
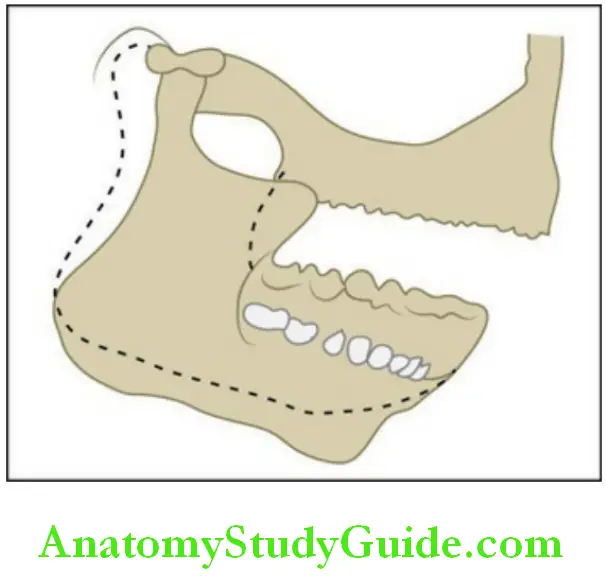
Translation:
- During wider mouth opening (12 mm) or excursive movements, the condyle glides forward in the synovial joint cavity between the superior surface of articular disc and the inferior surface of the glenoid fossa. This is called translatory movement.
2. Excursive movements
- Protrusion
- Retrusion
- Lateral excursion
These are opening, closing front, back and side-to-side movements of the mandible. These movements happen during mastication.
– When the mandible moves side to side, the particular side to which it moves is termed as the ‘working side’ or functioning side and the other side is called nonworking side or balancing side.
– When the mandible moves to the left side, then the left condyle is called working condyle and the right condyle will be nonworking condyle. The working side condyle will rotate in its axis or move laterally. This lateral movement is called lateral translation or ‘Bennet movement’. The joint movement occurs between the upper articular surface and the disc and also between the disc and mandibular head.
3. Other movements
- Functional movements
- Parafunctional movements
Temporomandibular Joint Dysfunction Symptoms
Functional movements are chewing, swallowing, yawning and other movements which take place within the border movements, that is, in extreme positions of the mandible in any direction which are limited by nerves, muscles and ligaments. Parafunctional movements of the mandible are the movements other than the normal movements such as bruxism, extremely wide opening of mandible during yawning.
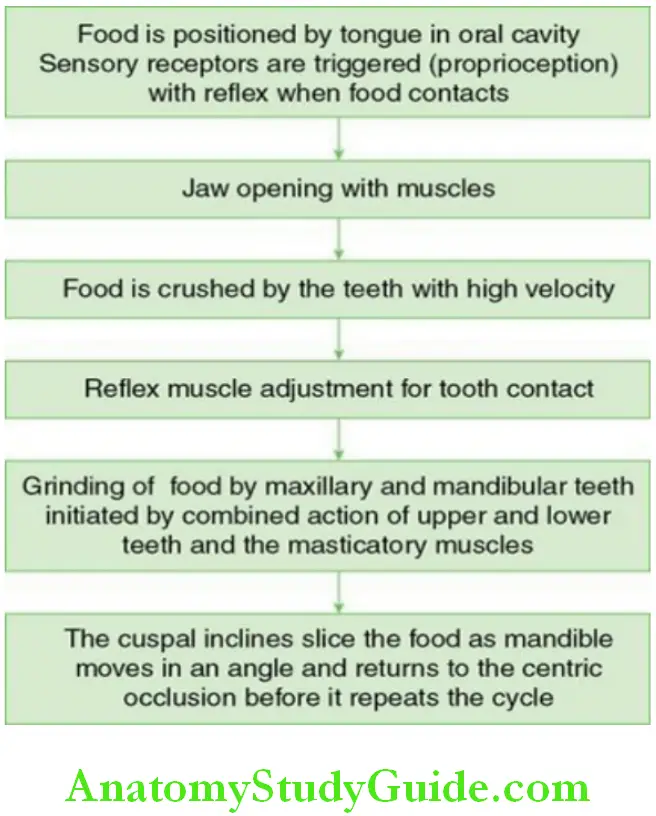
The Chewing Cycle
The chewing cycle or the masticatory cycle is the rhythmic movement of the mandible during mastication. When we record the envelope of motion during chewing, it forms a characteristic tear drop pattern in all the three planes. In adults when the food enters the mouth during chewing, the mandible moves forwards until the incisors meet and then the bolus moves towards the centre of the mouth. During that time, the mandible goes back to the original centric position. Then the side-to-side movement is initiated until the teeth contact.
The factors affecting the chewing cycle are:
- Consistency of the food
- Quantity of food
- Condition of the teeth
- Saliva
- Neuromuscular coordination
- Masticatory force
Murphy’s Masticatory Cycle
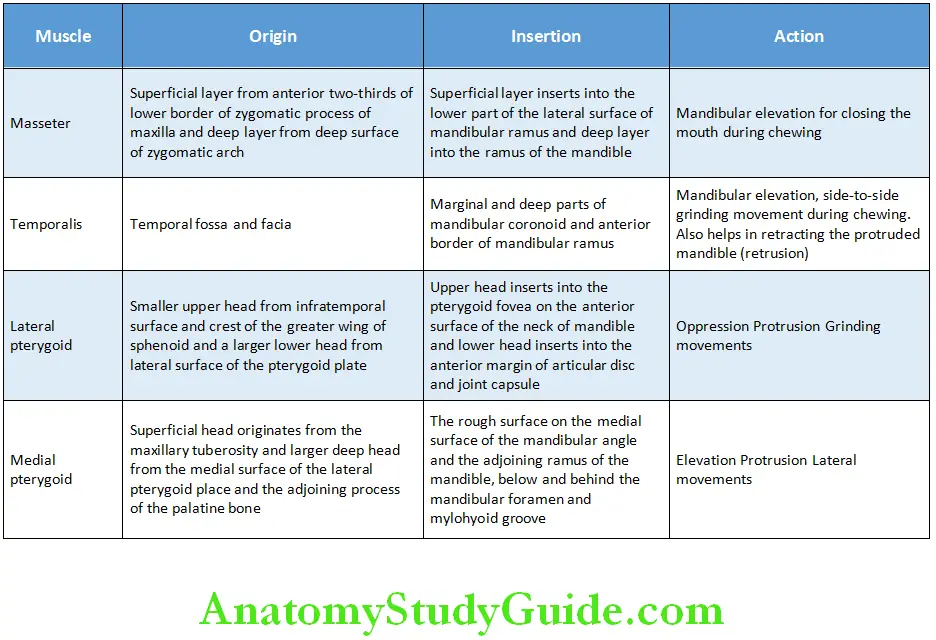
Associated Muscles Of The Temporomandibular Joint
The associated muscles of the TMJ are:
- Masseter
- Temporalis
- Lateral pterygoid
- Medial pterygoid
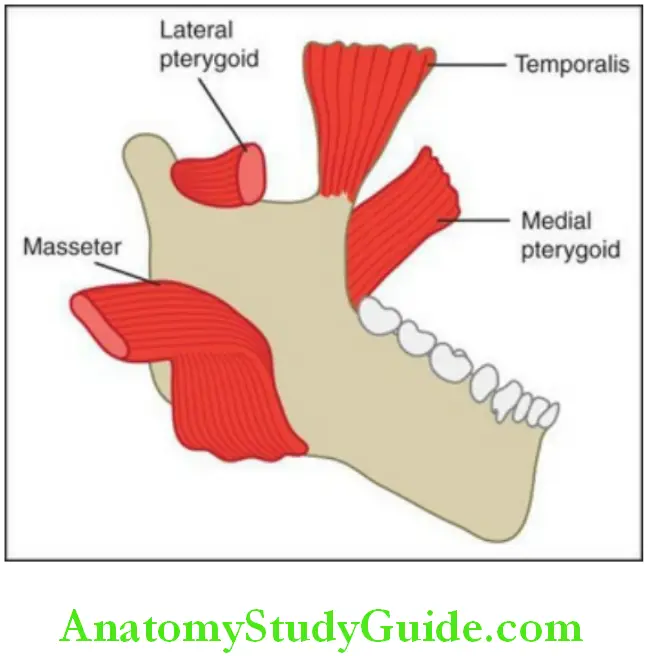
The origin, insertion and the actions of the muscles are mentioned in Table.
Muscles of theTemporomandibular Joint
Innervation And Blood Supply Of Temporomandibular Joint
- The four types of receptors are Ruffini corpuscles, Pacinian corpuscles, Golgi tendons and free nerve endings. They maintain the proprioception of the TMJ. These are innervated by auriculotemporal and masseteric branches of the mandibular nerve.
- The blood supply for the joint is predominantly provided by the superficial temporal artery and the maxillary artery.
Clinical Consideration Of TMJ
TMJ dislocation and displacement:
- During the excessive opening of the mouth while yawning or due to opening of mouth for longer time, the joint may dislocate anteriorly. This is also called luxation. This is often severely painful and can be repositioned and the condyle can be forced back to the joint by the surgeon under sedation. Sometimes habitual dislocation of the joint occurs in some individuals where they can reposition the joint themselves.
- In some cases, the condyle partially dislocates from the joint and this is called subluxation.
Temporomandibular Joint Anatomy – Ankylosis:
- Ankylosis is the stiffening or immobility of the joint which happens due to bony fusion or a result of a surgery. During TMJ ankylosis, the mouth opening is restricted which limits the jaw movements and leads to impaired speech. This is often painless.
Temporomandibular Joint Dysfunction Physical Therapy
Myofascial pain dysfunction syndrome (MPDS):
- Myofascial pain dysfunction syndrome is a psychological and physical disorder that may involve the joint and muscles which is often presented by dull radiating type of pain in the jaw.
- Various factors such as teeth loss, bruxism, bone resorption, poor fitting dentures, stress may contribute to this syndrome. The joint perse may not be involved.
- The treatment lies in careful differential diagnosis and behavioural modifications.
Clicking/snapping of Temporomandibular Joint
- During opening and closing of the jaw, sometimes there may be a clicking or snapping sound in the joint which is not normal. This could be due to muscular overcontraction.
- Prolonged clicking in the joint may damage the ligaments associated and the articular disc.
Components Of The Temporomandibular Joint
- Two bony structures
- Articular disc
- Fibrous capsule enclosing the joint
Features Of The Temporomandibular Joint
In the TMJ:
- The joint space is divided into the upper and lower compartments/joint cavities by an intraarticular disc.
- Upper joint cavity – gliding movements
- Lower cavity – hinge movements
- The articular surface is composed of fibrous tissue as the mandible develops from intramembranous ossification and there are no cartilages to cover the articular surface.
- Condylar cartilage which is a secondary cartilage of the mandible persists till adolescence
Articular Surfaces Of The Temporomandibular Joint
Mandibular condyle:
The head of the mandibular condyle in an adult is histologically made up of the following layers from superficial (articular surface) to the deep layer (bone of the condyle).
Fibrous tissue (articular surface layer):
- Fibrous tissue is the most superficial and is the articular surface.
- Majority are collagen fibres and some elastin fibres are also seen.
- Superficial layer – collagen fibres are parallel to the surface
- Deep layers – collagen fibres run vertically
- A few fibroblasts are also present.
Temporomandibular Joint Anatomy – Cell-rich layer/zone:
- Cell-rich layer is present below the articular surface.
- Highly cellular zone.
- Proliferation of cells occurs in this zone.
- This zone is a source for cells to replenish in the adjacent layers.
Fibrocartilaginous layer:
- Fibrocartilaginous layer is present below the cell-rich zone.
- As numerous cells are rounded and appear similar to cartilage like cells this layer is called fibrocartilaginous layer.
Temporomandibular Joint Dysfunction Physical Therapy
Calcified cartilage:
- The calcified cartilage covers the bone of the condyle.
- It is considered to be a remnant of the condylar cartilage which is a secondary cartilage of the mandible.
Articular surface of the mandibular fossa:
The articular surface of the mandibular fossa is similar to the condyle, except:
- The fibrous layer is thinner in the articular fossa and thick in the posterior region on the slope of the articular eminence.
- Crimping of the superficial collagen fibres is seen.
Condyle In A Child
Due to the appearance of the condylar cartilage in childhood, the histological appearance of the condyle varies with age. The cartilage appears in the 10th week of intrauterine life and lasts till adolescence.
Histology:
- The condyle is lined by fibrous tissue.
- The layer beneath is made of undifferentiated cells that later differentiate into chondrocytes to form the condylar cartilage.
– The cartilage is made up of type-II collagen. The chondrocytes in the deeper portion of the cartilage lay down type-X collagen, and subsequently, the matrix begins to ossify by endochondral ossification.
– After mineralization of the cartilage, the chondrocytes undergo apoptosis. A portion of the calcified cartilage is resorbed by osteoclasts.
– The osteoblasts lay down woven bone around the template of the calcified cartilage and this bone undergoes remodelling to form mature bone.
Intra-Articular Disc
The intra-articular disc contains cells which are embedded in a matrix comprising fibres and ground substance.
- Majority of the fibres are type I collagen fibres.
- Small quantities of other types of collagen are present.
- Traces of elastin is seen
- 80% of the disc is made up of water
Fibres:
Collagen Fibres:
- Type I collagen – 80% of dry weight of the articular disc
- Small quantities of Type III, VI, IX, XII are present.
- Traces of Type II collagen is seen due to the localized presence of fibrocartilage
Arrangement of collagen fibres in the disc:
- Thin central region also called the intermediate zone is present – the collagen fibres in this zone are thin and run anteroposteriorly.
- Thick anterior and posterior region – here the fibre bundles run transversely and superoinferiorly.
- Around the periphery – collagen fibres run circumferentially.
Temporomandibular Joint Dysfunction Physical Therapy
Elastin Fibres:
- Elastin fibres are present in the upper part of the disc.
- They decrease in number with age.
- Elastin fibres help in the recovery process postdisc loading or disc displacement.
Ground substance:
The ground substance comprises 5% of the dry weight.
It is made up of glycosaminoglycans (GAGs) including
- Chondroitin sulphate
- Dermatan sulphate and
- Traces of Heparan sulphate
GAGs absorb water and helps in adapting the disc to act as a shock absorber during compression on loading.
Cells:
- Cells are more at birth and decrease in number in the adult.
- The cells have an outline which is in between flat fibroblast like cells to round chondrocyte like cells.
- The cells have moderate number of organelle and considerable cytoplasm. The cells help in turnover of the extracellular matrix.
– When the cells of the disc secrete and turnover the collagen and ground substance and contain intracellular organelle, then these cells are called fibroblasts.
– When the cell synthesizes gap junction proteins and cause slow turnover of collagen, they are called fibrocytes.
The intra-articular disc has the following features:
- Proteoglycans containing high molecular weight chondroitin sulphate.
- Lack of/or traces of type II collagen fibres.
- Lack of pericellular matrix around the rounded cells with microvilli like processes that communicate with adjacent cells.
Blood and nerve supply:
- The blood vessels present in the disc at birth are lost immediately. The central portion and majority of the disc becomes avascular. The vessels are present only in the peripheral portion.
- In the bilaminar zone, the disc divides into the superior and inferior lamellae.
– Numerous vascular spaces are seen in the superior lamella. During mouth opening, blood flows into the back portion of the disc into the space behind the migrating condyle as the lateral pterygoid pulls the disc in a forward direction during mouth opening.
– The inferior lamella is comparatively avascular and inelastic.
Articular Capsule Of The Temporomandibular Joint
The articular capsule encloses the joint space. It is a dense collagenous sheet of tissue or a sac. It is made up of an outer layer of dense connective tissue and an inner layer lined by synovial membrane
Synovial Membrane Of The Temporomandibular Joint
The synovial membrane lines the inner surface of the fibrous capsule of the TMJ and the margins of the articular disc. The articular surfaces are not lined by synovial membrane as it could wear out
The synovial membrane consists of two layers of cells:
- Intimal layer which is cellular.
- Subintimal layer which is vascular.
- The intimal cells of the synovial membrane are of three types:
-
- Type B cells or fibroblast like cells rich in RER also called a secretory
S-cell - Type A cells or macrophage like cells rich in Golgi and lysosomes
- A cell with features intermediate to type B and A
- Type B cells or fibroblast like cells rich in RER also called a secretory
- The subintimal layer is made up of loose connective tissue comprising vessels, fibroblasts, macrophages. Collagen and elastin fibres are also seen.
- The synovial membrane shows periods of rest and metabolic activity and thus has regenerative capacity. It is folded in appearance at rest. These folds flatten out during jaw movements
Temporomandibular Joint Dysfunction Physical Therapy
Functions of the synovial membrane:
The membrane secretes a straw-coloured viscous synovial fluid present in the joint cavities, which helps in lubrication. The lubricating property of the joint is due to the presence of proteoglycans in the fluid. The amount of fluid secreted decreases with age.
Temporomandibular Joint Dysfunction Clinical Considerations
Disorders of the TMJ:
- Multifactorial in origin; common symptoms include
- Clicking of the joint
- Decreased mouth opening
- Pain in the joint, face or the region of the jaw
Fracture of the articular fossa:
- The thin nature of the bone in the articular fossa is liable to fracture in case of a blow to the condyle driving it into the fossa.
- The brain and dura matter may also be involved in such injuries.
Structural changes in the bone and fibrocartilaginous covering:
- Occurs after loss of posterior teeth leading to change in the forces and their direction.
- Fibrillation of the fibrous covering of the articular surfaces.
- Severe trauma might destroy the articular bone and cartilage leading to new bone formation in the marrow spaces and periphery of the condyle. This impairs the function of the joint.
Temporomandibular Joint Anatomy – Myofunctional pain dysfunction syndrome:
The main cause is the muscle spam and the condition is stress related. It is more common in females.
It is characterized by
- Tenderness of masticatory muscles
- Limited mouth opening
- Joint sounds
Treatment should be conservative.
Dislocation of the TMJ:
- Might occur even during yawning
- Usually bilateral and displaced anteriorly
Modification of the growth of the condylar cartilage:
- Early diagnosis of the imbalance in the growth of the maxilla and mandible leading to facial disharmony and occlusion can help in trying to modulate the growth of the condyle by orthodontic appliances.
– The appliance can be used to push the mandible behind and compress the condylar cartilage against the mandibular fossa to retard the growth of the mandible.
– Appliances can also be used to reposition the mandibular condyle forward to enhance the growth of the condyle in a forwardly direction.
Temporomandibular Joint Synopsis
- The TMJ also called the craniomandibular joint is the synovial articulation between the mandibular fossa in the temporal bone and the movable condyle of the mandible. It is a synovial joint and has a joint cavity filed with synovial fluid and thus allows considerable movement of the joint. The synovial fluid is secreted by the synovial membrane and lines the internal surface of the capsule of the joint.
- Components of the TMJ include two bony structures, an articular disc and a fibrous capsule enclosing the joint.
- The head of the mandibular condyle in an adult is histologically made up of of the following layers from superficial to the deep layers which are the fibrous tissue, cell-rich layer/zone, fibrocartilaginous layer, layer of calcified cartilage, bone of the head of the condyle.
- Articular surface of the mandibular fossa is similar to the condyle except that the fibrous layer is thinner in the articular fossa and thick in the posterior region on the slope of the articular eminence.
- Intra-articular disc contains cells which are embedded in a matrix comprising fibres and ground substance.
- The articular capsule encloses the joint space. It is a dense collagenous sheet of tissue or a sac. It is made up of an outer layer of dense connective tissue and an inner layer lined by synovial membrane.
- Synovial membrane lines the inner surface of the fibrous capsule of the TMJ and the margins of the articular disc. The articular surfaces are not lined by synovial membrane as it could wear out. The membrane secretes a straw-coloured viscous synovial fluid present in the joint cavities, which helps in lubrication. The lubricating property of the joint is due to the presence of proteoglycans in the fluid. The amount of fluid secreted decreases with age.
- The temporomandibular joint (TMJ) is the articulation between the temporal bone in the skull and the mandible. It is a diarthrodial and ginglymoid joint of synovial type.
- The components of the joint are glenoid fossae, articular eminence, articular capsule/temporomandibular ligament, articular disc, synovial cavity, accessory ligaments including stylomandibular ligament and sphenomandibular ligament and pterygomandibular raphae.
- TMJ plays an important role in the mandibular movements which are complex in nature. The different movements of the TMJ are basic movements which include rotation/hinge movement and translation. The other movements include functional and parafunctional movements.
- The associated muscles involved are essential for mastication. They are masseter, temporalis, lateral pterygoid and medial pterygoid.
Leave a Reply